Acute Low Back Pain in Children: A Guide to Diagnosis and Treatment
ABSTRACT: Unless the cause of back pain is obvious, order anteroposterior and lateral radiographs of the spine, a complete blood cell count, erythrocyte sedimentation rate, and urinalysis. If you suspect infection, tumor, or bony abnormalities, obtain an MRI scan or a CT scan. MRI has surpassed bone scanning as the gold standard for diagnosing spinal infections, because it confirms a specific anatomic diagnosis. Spondylolysis and spondylolisthesis are two of the most common causes of back pain in adolescents; the diagnosis is made with plain radiographs, which show slippage on the lateral view in patients with spondylolisthesis and fracture through the pars interarticularis on the oblique views in those with spondylolysis.
Key words: back pain, spondylolysis, spondylolisthesis, diskitis, osteomyelitis
Back pain in children—although relatively rare—is much more likely than it is in older persons to result from a serious diagnosable cause. Consequently, such pain requires a thorough investigation. Here, we describe what to look for when taking the history and conducting the physical examination. We also discuss appropriate tests and review the most common disorders in the differential.
INITIAL ASSESSMENT
History taking. Find out if there has been any change or increase in the patient’s activity level—in particular, participation in a new exercise regimen, gymnastics program, football, or dance. These activities raise the possibility of spondylolysis or spondylolisthesis.
Also ask if the patient has had any recent bacterial illness or fever, since bacteremia predisposes to spinal infection. Determine whether the gait has changed or activities have been voluntarily limited because of pain. Such a limitation is a major red flag. Pain that occurs at night or wakes the child from sleep suggests tumor or infection.
Physical examination. Three areas require thorough evaluation:
•In examining the skin, look for “birthmarks” (such as numerous café au lait spots) that may indicate neurofibromatosis and for midline abnormalities on the back, such as a hairy nevus, hemangioma, lipoma, or dermoid sinus. These lesions may sometimes indicate spina bifida or other spinal abnormalities.
•In examining the spine, note the amount of thoracic kyphosis and lumbar lordosis, and test for scoliosis. Scoliosis is a sign of a spinal disorder but is not usually the cause of the pain.
•Carefully observe the patient’s gait for any abnormalities.
Diagnostic evaluation. The initial evaluation of children with back pain is more comprehensive than that of adults. If the results of all diagnostic tests are unremarkable, monitor patients until their symptoms resolve.
Unless the symptoms have an obvious cause, obtain anteroposterior (AP) and lateral radiographs of the involved spine. Most pathology is visible on these initial views. Oblique views may be obtained if necessary, but only after review of the AP and lateral films, to limit the patient’s exposure to radiation.1
Routine laboratory testing includes a complete blood cell count, erythrocyte sedimentation rate (ESR), and urinalysis. Order an MRI scan or a CT scan to confirm any suspected infection, tumor, or bony abnormalities. Bone scans are valuable when you suspect tumor or infection in an infant or toddler but the affected area is difficult to locate. They may also reveal an early stress fracture or spondylolysis in an older child that is not evident on plain radiographs.
 DIFFERENTIAL DIAGNOSIS
DIFFERENTIAL DIAGNOSIS
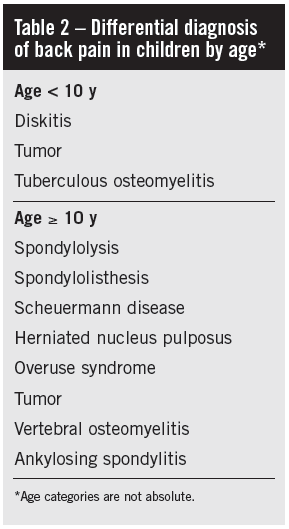
The differential diagnosis of pediatric back pain is extensive, but the various possible causes can be organized into four categories: mechanical disorders, developmental disorders, inflammatory processes, and neoplastic processes (Table 1).1 It may also be useful to organize the differential diagnosis according to age (Table 2).1 Age 10 appears to be a rational point to separate childhood conditions from those of adolescence. At about 18 years, the problems of adolescence begin to merge with those of adulthood.
 Diskitis. Infectious disorders are always a major concern in children with back pain. Intervertebral diskitis, presumed to be an infectious disorder, is often characterized as an acute inflammatory process without infection. The cause remains debatable because cultures of biopsy specimens from intervertebral disks are positive in only 25% of cases.1
Diskitis. Infectious disorders are always a major concern in children with back pain. Intervertebral diskitis, presumed to be an infectious disorder, is often characterized as an acute inflammatory process without infection. The cause remains debatable because cultures of biopsy specimens from intervertebral disks are positive in only 25% of cases.1
History and physical examination. Diskitis generally occurs in children younger than 10 years; the average age is 6 years.1 Patients present with a history of nonacute fever and an average of 5 weeks of ongoing symptoms. Older children usually have a history of limping and nonradiating back pain and stiffness. Younger children and toddlers may present with a limp, a refusal to walk or crawl, and abdominal pain or irritability.
The back examination may reveal anything from minimal findings to point tenderness over the lumbar spine, muscle spasm, loss of the normal lordotic curve of the lumbar spine, and a decreased range of motion of the spine secondary to pain.
Laboratory testing. Laboratory testing cannot always confirm a diagnosis of diskitis; the white blood cell (WBC) count is generally normal, and the ESR is elevated in only about 50% of patients.2 Blood cultures are generally obtained, but the results are almost always negative.
Early in the course of diskitis, plain radiographs are likely to be normal. However, as the disease progresses, they demonstrate narrowing of the disk space, end-plate irregularities, and erosion into the adjacent vertebral bodies. Bone scans are useful if there is ambiguity about the diagnosis or about the area of spinal involvement. However, MRI has surpassed bone scanning as the gold standard for evaluating spinal infections, because it confirms a specific anatomic diagnosis.3
 Treatment. The treatment of suspected diskitis includes hospital admission for bed rest, surveillance for possible infection, further diagnostic testing as needed and, possibly, antibiotics. The use of antibiotics for diskitis is controversial; however, if administered, the antibiotics should cover for Staphylococcus aureus. Obtain disk aspirates for culturing only if the diagnosis is in doubt or the patient fails to respond to conservative therapy.
Treatment. The treatment of suspected diskitis includes hospital admission for bed rest, surveillance for possible infection, further diagnostic testing as needed and, possibly, antibiotics. The use of antibiotics for diskitis is controversial; however, if administered, the antibiotics should cover for Staphylococcus aureus. Obtain disk aspirates for culturing only if the diagnosis is in doubt or the patient fails to respond to conservative therapy.
Vertebral osteomyelitis. The presentation of vertebral osteomyelitis is similar to that of diskitis; however, vertebral osteomyelitis—although sometimes seen in adolescents—usually occurs in adults. It is caused most commonly by S aureus; nonetheless, tuberculosis must also be considered in the differential diagnosis.
Diagnostic testing. The ESR and WBC count are invariably elevated, and blood cultures are frequently positive. Plain radiographs are usually normal early in the illness but within 3 to 4 weeks will demonstrate disk space narrowing, patchy osteoporosis of the involved vertebral body, or even vertebral collapse.2 MRI is the definitive imaging study.
Treatment. Hospitalization and intravenous antibiotic therapy are warranted. It may be prudent to delay antibiotic administration until the results of blood cultures and possibly needle biopsy of the affected vertebrae or abscess are obtained.2 Consultation with the spine surgeon is recommended before antibiotics are administered.
Spondylolysis and spondylolisthesis. These are 2 of the most common causes of back pain in adolescence.1 Spondylolysis is a defect or fracture through the pars interarticularis; spondylolisthesis involves the actual slippage of one vertebra onto another.
History and physical examination. These disorders are commonly found in gymnasts, dancers, and football players. Patients generally present with low back pain that is aggravated by activity and at least partially relieved by rest. The physical examination may show tenderness over the lower spine, possibly with a palpable step-off of L5 shifting forward on S1.
Almost 90% of spondylolysis occurs at the L5 level, and more than 96% occurs at either L4 or L5.4 In addition, there may be hamstring tightness or spasm. Neurologic abnormalities are unusual. The one-legged lumbar extension maneuver is a fairly sensitive indicator of disease. To do this test, the patient stands on one leg and extends backward. Spondylolysis frequently causes ipsilateral pain.4
Diagnostic evaluation and treatment. The diagnosis is made with plain radiographs, which show the slippage on the lateral view in patients with spondylolisthesis and the fracture through the pars interarticularis on the oblique views in those with spondylolysis (Figure). Oblique views are necessary to detect spondylolysis; without them, up to 20% of these injuries will be missed.4 If radiographs are normal but the patient is still felt to be at high risk, a bone scan is a very sensitive means to detect the injury. Treatment is conservative and symptomatic; it involves restricting painful activity and, occasionally, initiating physical therapy. Surgery is restricted to patients who do not respond to conservative care.
 REFERENCES:
REFERENCES:
1. King H. Back pain in children. Pediatric Clin North Am. 1984;31:1083-1095.
2. Krug S. Back pain in children. In: Reisdorff E, Roberts M, Wiegenstein J, eds. Pediatric Emergency Medicine. Philadelphia: WB Saunders Co; 1994: 983-991.
3. Rothman S. The diagnosis of infections of the spine by modern imaging techniques. Orthop Clin North Am. 1996;27:15-31.
4. Garry J. Lumbar spondylolysis in adolescent athletes. J Fam Pract. 1998;47:145-149.
5. Sasso R, Cotler HB, Guyer RD. Evaluating low back pain: the role of diagnostic imaging.
J Musculoskel Med. 1991;8(5):21-37.
The opinions and assertions contained herein are the private views of the authors and should not be construed as official or as reflecting the views of the Department of the Army or the Department of Defense.


