Acutely Traumatized Children: Identifying and Managing Posttraumatic Stress
ABSTRACT: Pediatric providers play a vital role in identifying and providing care (directly or by referral to specialists) to traumatized children and their families. However, children exposed to traumatic violence, disasters, or life-threatening accidents that occur on an everyday basis often are not detected in the course of routine pediatric care. Whether psychological trauma occurs in a highly visible event, such as the recent Sandy Hook Elementary School shooting, or in the course of children’s daily lives, pediatric providers are confronted with a dual challenge: identifying children who have or are at risk for posttraumatic stress impairment, and providing those children and their caregivers with immediate help and access to appropriate care. This article describes an evidence-based, practical approach for pediatric practitioners, summarized by the mnemonic STAGE: surveillance, trauma-informed anticipatory guidance, and evaluation to plan treatment and coordinate referrals. Practical suggestions and resources are offered to enable providers to apply the STAGE approach to caring for traumatized children and their caregivers within the constraints of real-world pediatric practice.
How can you speak to children and parents in the wake of unspeakably traumatic events?
Every day, in every community, children are exposed to traumatic threats to their safety, health, and relationships.1 Public and professional awareness about children’s exposure to violence has been heightened by recent events such as the Sandy Hook Elementary School shooting in Newtown, Connecticut. The shattering impact that natural disasters such as hurricanes, earthquakes, and tornadoes can have on the lives of children and families also has become widely recognized. Yet these highly publicized traumatic events are only the tip of the iceberg: Thousands of children are exposed every day to potentially traumatic stressors such as physical and sexual abuse; family, community, and school violence; bullying; and life-threatening or severely injurious disasters, accidents and illnesses. Children exposed to these stressors often unnoticed or are treated only for physical injuries.
Pediatric practitioners can identify traumatized children and their families and provide or arrange for the care they need in order to recover psychologically and physically from traumatic exposures.2-4 Cohen and colleagues provide an excellent introduction to the issues and resources available to pediatricians for identifying, treating, and referring traumatized children.5 They describe 2 brief screening questionnaires for parents and children that can be used to identify prominent posttraumatic stress disorder (PTSD) symptoms, and they offer examples of how to sensitively ask a child or parent whether potentially traumatic events have occurred in the child’s recent life. They also describe evidence-based psychotherapies to which pediatric practitioners can refer patients for mental health evaluation and treatment of possible PTSD.
A recent survey found that pediatricians identified less than 10% of patients with trauma-related psychological problems.6 Only 18% of the surveyed pediatricians viewed themselves as having adequate knowledge of childhood PTSD, and less than 15% reported frequently asking about and identifying patients’ potential traumatic events in the past year or assessing and treating posttraumatic stress symptoms. Thus, despite the availability of evidence-based trauma and PTSD screening tools and treatments, there appears to be a need among pediatric providers to increase the recognition of and provide services for the traumatized children whom they see.7,8
Doing so requires attention to the practical barriers that pediatricians can face when attempting to address all of their patients’ medical and psychological risks and problems. First, there is the accurate identification of traumatized children within the scope of pediatric practice: Even brief screening measures may require more time than is feasible to administer and to follow up on. Second, following up on screening requires not only added time, but also skill in evaluating the trauma-related needs of the child and family and advising and educating parents so as to increase their confidence and ability to help their traumatized child. In addition to awareness of evidence-based PTSD screening tools and treatments, pediatric providers need practical guidance about how to identify traumatized children in the course of routine practice, and how to provide immediate help to those children and their caregivers.
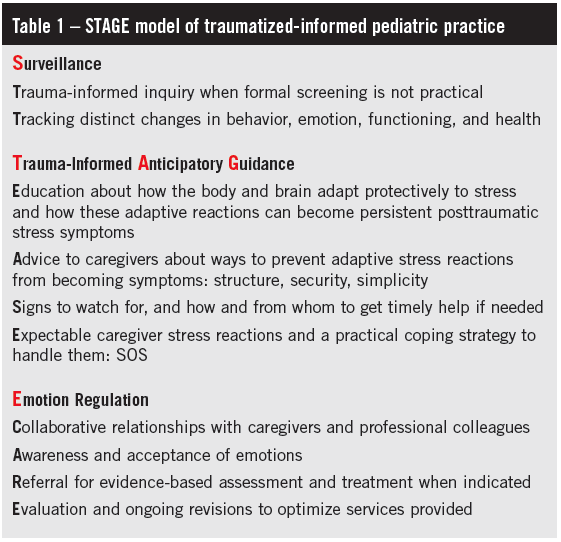
To that end, this paper builds upon Cohen and colleagues’ foundational article,5 offering practical guidelines for helping traumatized children, based on the mnemonic STAGE: surveillance, trauma-informed anticipatory guidance, and emotion regulation (Table 1).
Step 1: Surveillance
Children are exposed to a wide variety of traumatic stressors, and they experience a correspondingly wide variety of posttraumatic psychosocial impairments.1 To adapt a familiar aphorism, “When you have seen one traumatized child, you’ve seen one traumatized child.” It is neither scientifically nor clinically justified to take a one-size-fits-all approach with traumatized children. However, it is not practical for pediatric providers to assess every potentially traumatic event that their patients have ever experienced. An alternative is to routinely ask parents or caregivers while getting the history whether the child has experienced or witnessed any extremely stressful events. It also is important to ask parents whether they or other family members have had life-threatening or extremely stressful experiences (eg, domestic violence9), in order to identify events that may have been indirectly traumatic for the child, even if the child was not directly physically harmed.
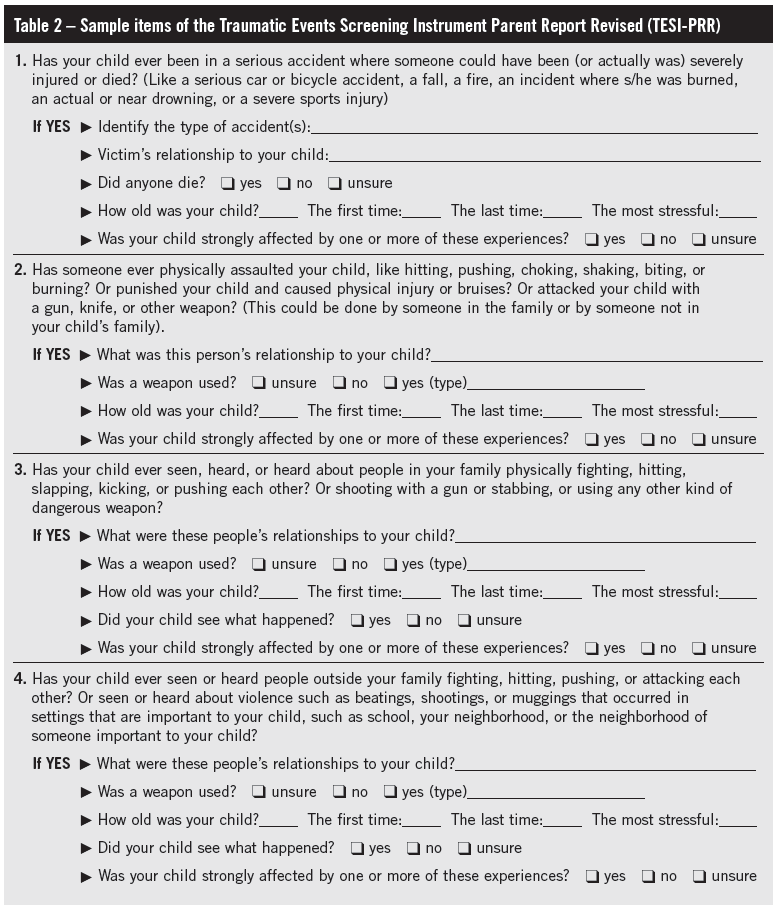
Although this strategy is efficient and generally well accepted by parents, 3 caveats should be noted. First, caregivers have highly variable personal definitions for what constitutes a life-threatening or extremely stressful event. Therefore, in order to evaluate whether the reported events may have been traumatic, it is helpful to refer to a carefully constructed and thorough trauma-screening instrument, such as the Traumatic Events Screening Instrument (Table 2). Such screening tools will be most useful to pediatric providers as a framework for selective inquiry about specific events rather than as an omnibus screening interview. For example, if a parent reports that a child has been “abused,” the pediatric provider can briefly clarify the nature of the maltreatment (eg, sexual, physical, emotional; severe neglect) using the down-to-earth behavioral language provided by the trauma screening items. The trauma screening questions can guide pediatric providers as they accurately translate parents’ vague terms such as abuse into very specific forms of potentially traumatic injury, victimization, or loss.
(Click to enlarge)
The second caveat is that parents may be unaware of or reluctant to disclose potentially traumatic events that have happened to their child. Moreover, most children who experience potentially traumatic events do not develop lasting debilitating posttraumatic stress problems,10 while some children develop posttraumatic stress problems despite their caregivers not being aware of any traumatic exposures.11 Therefore, in addition to identifying children’s potentially traumatic experiences, it also is essential to determine whether the child is now experiencing posttraumatic symptoms or is at risk for persistent posttraumatic distress.12-14 Traumatic stress can alter children’s development in a variety of ways not limited to the anxiety and dysphoria related to distressing memories.15,16 Pediatric providers therefore should be alert to the emergence or intensification of a wide variety of problems that may be related to traumatic stress dysregulation in a child who has experienced adversity (Table 3). None of these problems are definitive evidence of trauma exposure or traumatic stress symptoms, but their appearance or exacerbation should alert the practitioner to be watchful for indications that the child has experienced traumatic stress and may need specialized treatment for posttraumatic stress.
 Step 2: Trauma-Informed Anticipatory Guidance
Step 2: Trauma-Informed Anticipatory Guidance
The third caveat regarding care of traumatized children is that when a pediatric provider identifies a potentially traumatized child, he or she has the immediate responsibility of providing assistance to the child and parents. Combining the best practice approach of anticipatory guidance with a trauma-informed framework offers a practical solution to this critical challenge.
Anticipatory guidance involves determining parents’ questions, concerns, and desired information (eg, developmental and behavioral milestones17), and then providing it in a way that enables parents to confidently make and act on decisions about their child’s health. This stands in sharp contrast to merely offering generic advice about parenting, which 1 study found was not desired by (and might undermine the working alliance with) an ethnoculturally diverse sample of parents.18 Although no published studies have investigated anticipatory guidance for traumatized children, clinical practice suggests 4 components, delineated by the acronym EASE (Table 1).
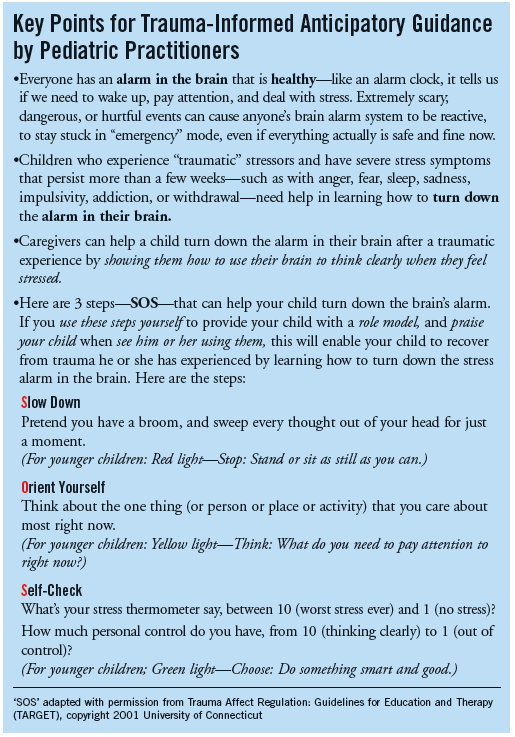
Education for both the child and the caregiver about the impact of psychological trauma and symptoms of PTSD is the first step in evidence-based treatment for traumatized children.5 Helping parents and children understand PTSD symptoms as the body and brain’s way of gearing up or shutting down to deal with situations involving extreme stress or danger can reduce the stigma and helplessness that traumatized children and their parents often feel. (The Box lists sample key points for trauma-informed educational anticipatory guidance.)
Parents often seek advice about helping their child manage traumatic stress reactions. Parents have varying degrees of knowledge about how to parent (or teach, or discipline) their child, which they tend to want to have affirmed rather than critiqued.6 Few parents are prepared for the challenges and responsibilities of caring for a traumatized child. The point of advice most consistently offered in fact sheets for families with traumatized children is that parents maintain or reinstate and strengthen daily routines to provide security and structure for their children, outside the home (eg, at school or in activities) as well as within the family.
Helping parents to distinguish nonclinical (eg, transient, mildly impairing) signs and symptoms from severe traumatic stress symptoms is a third key element in trauma-informed anticipatory guidance. Educational resources have been developed specifically to help pediatric providers educate caregivers about pediatric PTSD symptoms, when to seek specialized services, and the core elements in evidence-based psychosocial treatments for traumatized children.19
Expectable parent stress reactions, and practical guidance for handling them, often are an unacknowledged subtext in pediatric visits. Parents are profoundly affected when their child has been traumatized, and their ability to regulate their own emotions plays an essential role in their child’s recovery.20 Parents also may be trauma survivors themselves, either along with their child (eg, in cases of domestic violence) or separately (eg, trauma in their own childhoods). Evidence-based interventions have been developed specifically to enable traumatized parents to successfully regulate their emotions and recover from primary or secondary traumatic stress,21 but pediatric providers can directly facilitate this by teaching parents (and children) practical skills for regulating emotions (eg, “SOS,” Box).
Step 3: Emotion Regulation
Pediatric providers being attuned to stress-related fluctuations in their own emotions—which are expectable in health care encounters, especially those involving traumatized patients and caregivers—reduces that chance of adding further stress to patients or parents who are already distressed and emotionally dysregulated due to traumatic events.22
Good professional self-care is important not only to maintain pediatric providers’ health and effectiveness, but also to provide a role model for emotion regulation and a source of relational security for traumatized children and their parents. This self-care is based on developing a combined personal and professional approach to emotion regulation, which does not require pediatric providers to get specialized professional training or personal psychotherapy.
As noted in Table 1, 4 sources of emotion regulation are essential for every pediatric provider, as summarized by the acronym CARE (collaboration, awareness, referral, and evaluation). A collaborative approach to building and maintaining relationships with parents and professional colleagues not only is consistent with best practice research,23 but also strengthens the pediatric practitioner’s professional social support system. Practitioner awareness and acceptance of emotions is an application of the mindfulness approach to health care that can enhance collaboration and a positive provider-patient alliance.24 Judicious referrals of traumatized children and parents to specialists who can conduct evidence-based specialized assessment and treatment25 is another way to extend the pediatric practitioner’s professional support network. Finally, ongoing evaluation and performance-based revision of services provided to traumatized children and their parents not only optimize practitioners’ effectiveness but also enable them to confidently determine the limits of their expertise in assessing and treating traumatized children. Thus, simply by purposefully applying best practice guidelines, pediatric practitioners can enhance their own emotion regulation, well-being and effectiveness, thus serving as a role model and facilitator of emotion regulation for the traumatized children and their parents whom they see in their practice.
Conclusion
Treating traumatized children in pediatric practice poses a number of daunting challenges in addition to the ones inherent in providing “usual” pediatric care. However, applying some straightforward practical guidelines for surveillance, trauma-informed anticipatory guidance, and emotion regulation, a pediatric provider can accomplish a great deal on behalf of traumatized patients and their parents within the constraints of daily practice. In combination with the PTSD-related resources for screening and treatment described by Cohen and colleagues,5 the STAGE model for trauma-informed pediatric care offers a practical approach for pediatric providers to make a key difference in the lives of traumatized children whom they see in their practices.
References:
1. Fairbank JA, Fairbank DW. Epidemiology of child traumatic stress. Curr Psychiatry Rep. 2009;11(4):289-295.
2. Hagan JF Jr; American Academy of Pediatrics Committee on Psychosocial Aspects of Child and Family Health; Task Force on Terrorism. Psychosocial implications of disaster or terrorism on
children: a guide for the pediatrician. Pediatrics. 2005;116(3):787-795.
3. American Academy of Pediatrics Task Force on Violence. The role of the pediatrician in youth
violence prevention in clinical practice and at the community level. Pediatrics. 1999;103(1):
173-181.
4. American Academy of Pediatrics; Pediatric Orthopaedic Society of North America. Management of pediatric trauma. Pediatrics. 2008;121(4):849-854.
5. Cohen JA, Kelleher KJ, Mannarino AP. Identifying, treating, and referring traumatized children: the role of pediatric providers. Arch Pediatr Adolesc Med. 2008;162(5):447-452.
6. Banh MK, Saxe G, Mangione T, Horton NJ. Physician-reported practice of managing childhood posttraumatic stress in pediatric primary care. Gen Hosp Psychiatry. 2008;30(6):536-545.
7. Sabin JA, Zatzick DF, Jurkovich G, Rivara FP. Primary care utilization and detection of emotional distress after adolescent traumatic injury: identifying an unmet need. Pediatrics. 2006;117(1):
130-138.
8. Steen RG, Hamer RM. Stressing about posttraumatic stress disorder [letter]. Pediatrics. 2007;
120(1):232-234.
9. Thackeray JD, Hibbard R, Dowd MD; Committee on Child Abuse and Neglect; Committee on Injury, Violence, and Poison Prevention. Clinical report—intimate partner violence: the role of the pediatrician. Pediatrics. 2010;125(5):1094-1100.
10. Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Arch Gen Psychiatry. 2007;64(5):577-584.
11. Copeland WE, Keeler G, Angold A, Costello EJ. Posttraumatic stress without trauma in children. Am J Psychiatry. 2010;167(9):1059-1065.
12. Kenardy JA, Spence SH, Macleod AC. Screening for posttraumatic stress disorder in children
after accidental injury. Pediatrics. 2006;118(3):1002-1009.
13. Steinbaum DP, Chemtob C, Boscarino JA, Laraque D. Use of a psychosocial screen to
detect children with symptoms of posttraumatic stress disorder: an exploratory study. Ambul
Pediatr. 2008;8(1):32-35.
14. Winston FK, Kassam-Adams N, Garcia-España F, Ittenbach R, Cnaan A. Screening for risk of
persistent posttraumatic stress in injured children and their parents. JAMA. 2003;290(5):643-649.
15. Briggs-Gowan MJ, Carter AS, Clark R, Augustyn M, McCarthy KJ, Ford JD. Exposure to potentially traumatic events in early childhood: differential links to emergent psychopathology. J Child Psychol Psychiatry. 2010;51(10):1132-1140.
16. Ford JD, Gagnon K, Connor DF, Pearson G. History of interpersonal violence, abuse, and nonvictimization trauma and severity of psychiatric symptoms among children in outpatient psychiatric treatment. J Interpers Violence. 2011;26(16):3316-3337.
17. Dworkin PH. Detection of behavioral, developmental, and psychosocial problems in pediatric primary care practice. Current Opin Pediatr. 1993;5(5):531-536.
18. Dumont-Mathieu TM, Bernstein BA, Dworkin PH, Pachter LM. Role of pediatric health care professionals in the provision of parenting advice: a qualitative study with mothers from 4 minority ethnocultural groups. Pediatrics. 2006;118(3):e839-e848.
19. Trauma screening, identification and referral in pediatric practice. Educating Practices in the Community (EPIC) Program. Farmington, CT: Child Health and Development Institute of Connecticut. http://www.chdi.org/ourwork-signature-epic-publications.php?page=18. Accessed March 8, 2013.
20. Ostrowski SA, Ciesla JA, Lee TJ, Irish L, Christopher NC, Delahanty DL. The impact of caregiver distress on the longitudinal development of child acute post-traumatic stress disorder symptoms
in pediatric injury victims. J Pediatr Psychol. 2011;36(7):806-815.
21. Ford JD, Steinberg KL, Zhang W. A randomized clinical trial comparing affect regulation and social problem-solving psychotherapies for mothers with victimization-related PTSD. Behav Ther. 2011;42(4):560-578.
22. Ford JD, Cloitre M. Best practices in psychotherapy for children and adolescents. In: Courtois CA, Ford JD, eds. Treating Complex Traumatic Stress Disorders: An Evidence-Based Guide.
New York, NY: Guilford Press; 2009:59-81.
23. Sharek PJ, Mullican C, Lavanderos A, et al. Best practice implementation: lessons learned from
20 partnerships. Jt Comm J Qual Patient Saf. 2007;33(12 suppl):16-26.
24. Conboy LA, Macklin E, Kelley J, Kokkotou E, Lembo A, Kaptchuk T. Which patients improve: characteristics increasing sensitivity to a supportive patient-practitioner relationship. Soc Sci Med. 2010;70(3):479-484.
25. Ford JD, Courtois CA, eds. Treating Complex Traumatic Stress Disorders in Children and
Adolescents: Scientific Foundations and Therapeutic Models. New York, NY: Guilford Press; 2013.