Are These Lumps and Bumps a Cause for Concern?
Cephalohematoma
A newborn infant presented with localized swelling in the right parietal area. He was born to a 20-year-old gravida I, para 0 mother following a difficult forceps delivery. Birth weight and length were 3.2 kg and 51.5 cm, respectively. Apgar scores were 5 and 7 at 1 and 5 minutes, respectively. On physical examination, swelling in the right parietal area was noted. The swelling was soft and fluctuant and did not transilluminate. This infant has cephalohematoma.

A cephalohematoma is a collection of blood between the pericranium and the skull. The hematoma almost always is limited by the periosteal attachments at the suture lines. It is rare that a cephalohematoma crosses a synostosed sagittal suture.1 The swelling often is not evident at birth but usually presents within the first 24 to 72 hours after delivery.2 The lesion is soft and fluctuant. The site of predilection is the parietal area, possibly because it is the most prominent presenting point.1,2
Cephalohematomas occur in approximately 1% to 2% of spontaneous vaginal deliveries and approximately 4% of vacuum-assisted or forceps deliveries.3 The lesion may result from an injury to the fetal head as it is forced through the birth canal, especially if the labor is difficult or prolonged.4 The condition is more common in primigravidas and in large infants.5 For unknown reasons, it is 2 times more common in male infants than in female infants.5 Infants may develop a late cephalohematoma following craniofacial surgery.6 Cephalohematomas may be unilateral or bilateral.1 Linear skull fractures occur in approximately 5% of unilateral and 18% of bilateral cephalohematomas.5
Most neonatal cephalohematomas are asymptomatic and usually reabsorb over time without sequelae.2 However, larger cephalohematomas may cause anemia and hyperbilirubinemia. In rare cases, cephalohematomas become infected either hematogenously or by contiguous spread of infection.4 Peripheral calcification may develop if the lesion persists beyond 4 weeks.5 In a small percentage of cases, it can lead to significant asymmetry and deformity of the skull.2
REFERENCES:
1. Currarino G. Neonatal subperiosteal cephalohematoma crossing a synostosed sagittal suture. Pediatr Radiol. 2007;37(12):1283-1285.
2. Kortesis BG, Pyle JW, Sanger C, Knowles M, Glazier SS, David LR. Surgical treatment for scaphocephaly and a calcified cephalohematoma. J Craniofac Surg. 2009;20(2):410-413.
3. Weiss KJ, Edwards MS, Hay LM, Allen CH. Escherichia coli-infected cephalohematoma in an infant. Clin Pediatr (Phila). 2009;48(7):763-766.
4. Kersten CM, Moellering CM, Mato S. Spontaneous drainage of neonatal cephalohematoma: a delayed complication of scalp abscess. Clin Pediatr (Phila). 2008;47(2):183-185.
5. Nicholson L. Caput succedaneum and cephalohematoma: the Cs that leave bumps on the head. Neonatal Netw. 2007;26(5):277-281.
6. Ghali S, Knox KR, Boutros S, Thorne CH, McCarthy JG. The incidence of late cephalohematomas following craniofacial surgery. Plast Reconstr Surg. 2007;120(4):1004-1008.
Caput Succedaneum
This infant was born at term to a 22-year-old gravida I, para 0 mother after an uncomplicated pregnancy. Vacuum extraction was used because of fetal distress. Apgar scores were 7 and 9 at 1 and 5 minutes, respectively. Birth weight and length were 2.9 kg and 50 cm, respectively. At birth, a mass was noted on the vertex. On physical examination, there was a soft swelling at the vertex of the skull. Subconjunctival hemorrhage was noted in both eyes. The rest of the physical examination findings were normal.
The infant has a caput succedaneum. A caput succedaneum presents as a diffuse swelling of the soft tissue of the scalp involving the presenting part of the fetus during delivery. It is most frequently seen on the vertex and the occipital midline of the head.1,2 The swelling is pitting in nature, is not sharply defined, and may extend across suture lines.1 Discoloration of the scalp may occur secondary to petechiae and/or ecchymosis. The size of the swelling is maximal at birth.

Caput succedaneum may develop secondary to injury to the presenting fetal head during a difficult or prolonged labor or during vacuum extraction or forceps delivery. The swelling results from the uterine, cervical, and vaginal pressure on the infant’s head, which causes exudation/extravasation of serosanguineous fluid into the subcutaneous tissue above the periosteum.2,3 The condition is more common in a primigravida and in cases of premature rupture of membranes.4
A caput succedaneum usually resolves within a few days.3 Oxygen saturation readings from the caput succedaneum are consistently lower than in the unaffected areas of the newborn’s scalp.5 Halo scalp ring, a type of alopecia, is an uncommon complication of caput succedaneum, presumably resulting from pressure necrosis of the neonatal scalp tissue.3,4 It is unusual for skull fracture and subaponeurotic hemorrhage to be associated with a caput succedaneum.3
REFERENCES:
1. Gerscovich EO, McGahan JP, Jain KA, Gillen MA. Caput succedaneum mimicking a cephalocele.
J Clin Ultrasound. 2003;31(2):98-102.
2. Nicholson L. Caput succedaneum and cephalohematoma: the Cs that leave bumps on the head. Neonatal Netw. 2007;26(5):277-281.
3. Neal PR, Merk PF, Norins AL. Halo scalp ring: a form of localized injury associated with caput succedaneum. Pediatr Dermatol. 1984;2(1):52-54.
4. Martín JM, Jordá E, Alonso V, Villalón G, Montesinos E. Halo scalp ring in a premature newborn and review of the literature. Pediatr Dermatol. 2009;26(6):706-708.
5. Johnson N, Johnson VA, Bannister J, Lilford RJ. The effect of caput succedaneum on oxygen saturation measurements. Br J Obstet Gynaecol. 1990;97(6):493-498.
GANGLION
A 16-year-old girl was noted to have a mass at the ventral aspect of the left wrist. The mass was asymptomatic and tensely cystic. There was no history of trauma.
A ganglion is a cystic swelling that typically arises from the synovium of either a joint capsule or a tendon sheath. The cyst contains a clear, gelatinous, colloid material or a thick, mucinous fluid. The latter contains hyaluronic acid and other mucopolysaccharides.1 The fluid is surrounded by a dense network of collagen fibers and fibrocytes.1 The most common sites include the dorsum of the wrist and the dorsum of the foot, although ganglion cysts may occur throughout the body. Ganglion cysts seldom emanate from within a joint itself; the incidence of intra-articular lesions has been reported to be 0.2% to 1.6% on magnetic resonance imaging scans.2 Ganglia often are asymptomatic. Occasionally, localized pain, paresthesia, limitation of motion, or weakness of the involved area may occur.1 The condition can be complicated by carpal tunnel syndrome.3

Because most cases resolve spontaneously, no treatment is necessary. Treatment with needle aspiration or surgical excision is indicated only if the ganglion is large, causes pain, or interferes with normal tendon function.
REFERENCES:
1. Sloane J, Gulati V, Penna S, Pastides P, Baghla DP. Large intra-articular anterior cruciate ligament ganglion cyst, presenting with inability to flex the knee. Case Rep Med. 2010;2010:705919.
2. Derman P, Kamath AF, Kelly JD IV. Ganglion cysts of the posterior cruciate ligament. Am J Orthop (Belle Mead NJ). 2011;40(5):257-258.
3. Shimizu A, Ikeda M, Kobayashi Y, Saito I, Oka Y. Carpal tunnel syndrome caused by a ganglion
in the carpal tunnel with an atypical type of palsy: a case report. Hand Surg. 2011;16(3):339-341.
PREAURICULAR FIBROMA
A 2-year-old girl presented with a soft-tissue mass in the right preauricular area. The mass was asymptomatic and had been present since birth. The child was born to a 23-year-old, gravida II, para I mother. Maternal health was unremarkable, and the mother was not on any medication during the pregnancy. There was no history of trauma.
The girl has a preauricular fibroma. A fibroma is the most common fibrous lesion of the skin. The lesion is soft and either skin-colored or slightly hyperpigmented. Histologically, the lesion consists of loose to dense collagenous stroma with thin-walled dilated blood vessels in the center.
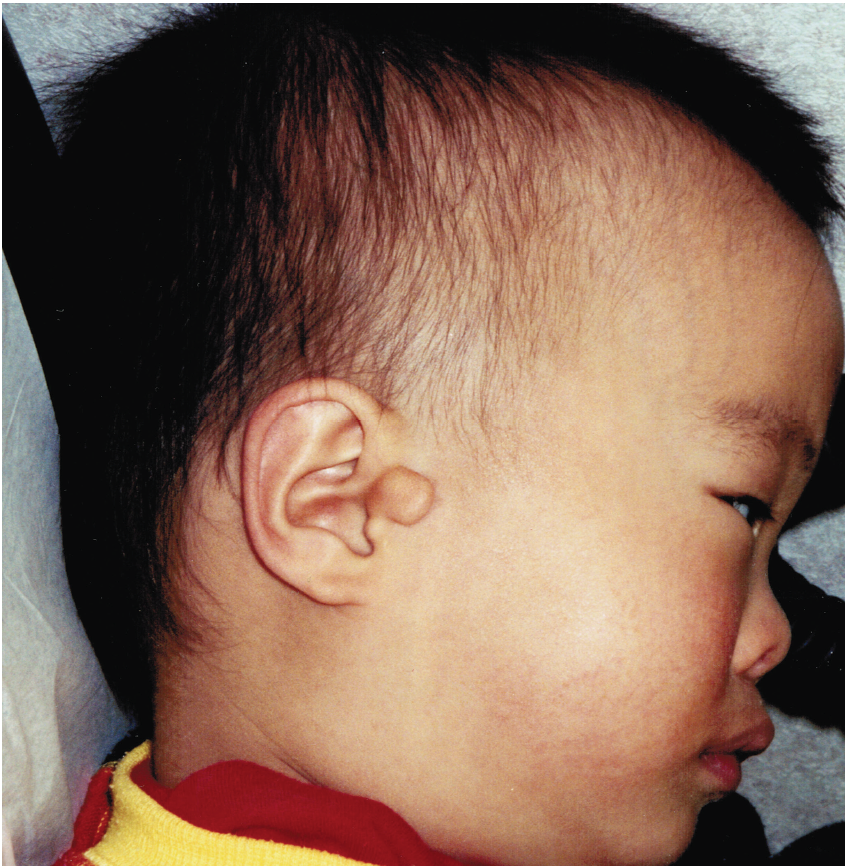
In most cases, preauricular fibromas have no clinical significance. However, they are found with increased frequency in cat-eye syndrome, Kabuki make-up syndrome, Melnick-Fraser syndrome, Cowden disease, and oculoauriculovertebral dysplasia.1
Excision of the lesion may be considered for cosmetic purposes.
REFERENCE:
1. Amer M, Mostafa FF, Attwa FM, Ibrahim S. Cowden’s syndrome: a clinical, immunological, and histopathologic study. Int J Dermatol. 2011;50(5):516-521.
MIKULICZ SYNDROME
A 3-year-old boy presented with a 3-month history of bilateral, painless submandibular masses, more obvious on the left side. He also complained of dry mouth and dry eyes. He did not have fever, respiratory symptoms, night sweats, a decrease in appetite, weight loss, rash, joint pain, or joint swelling. His past medical history was unremarkable. There was no family history of tuberculosis, collagen vascular disease, or lymphoproliferative disease.
Mikulicz syndrome (benign lymphoepithelial lesion) is an autoimmune disorder characterized by diffuse and bilateral enlargement of salivary and lacrimal glands with characteristic histopathologic findings, including diffuse lymphocytic infiltration of the exocrine glands and formation of epimyoepithelial islands.1-3

The usual clinical picture is enlargement of 1 or more of the salivary glands and, less frequently, the lacrimal glands.1 The condition often is bilateral and symptomless. Occasionally, mild local discomfort may be associated. The parotid glands usually are affected. Enlargement of lacrimal glands may result in a bulge below the outer ends of the eyelids and narrowing of the palpebral fissures. Depending on the degree of involvement, some patients may have xerostomia and xerophthalmia. Characteristically, patients are not thirsty despite xerostomia.1
Mikulicz syndrome may be primary (idiopathic) or may be caused by an underlying disease. A primary benign lymphoepithelial lesion without a specific underlying cause is a clinical rarity,3,4 occurring predominantly in middle-aged or older women but also possibly occurring in children.2
Secondary causes include Sjögren syndrome, which is characterized by xerostomia, keratoconjunctivitis, and a collagen vascular disease—usually rheumatoid arthritis, systemic lupus erythematosus, systemic sclerosis, or polymyositis.1 Rarely, Mikulicz syndrome occurs in association with tuberculosis, syphilis, sarcoidosis, AIDS, leukemia, lymphomas, or thiouracil treatment.1,5
Typical sonographic findings include hypoechoic areas with relatively high vascularization in the affected salivary glands.5
The diagnosis can be confirmed with a biopsy of the involved gland. Histologically, a benign lymphoepithelial lesion is characterized by atrophy of the acinar tissue with diffuse lymphocytic infiltration, and an intraductal proliferation of epithelial and myoepithelial cells with the formation of epimyoepithelial islands.1,5
A complete blood count is useful if infection is suspected. Erythrocyte sedimentation rate, serum immunoglobulins, rheumatoid factor, antinuclear antibodies, and autoantibodies to nucleoprotein antigens (SSA [Ro] and SSB [La]) should be considered if Sjögren syndrome is suspected. A Mantoux test is helpful if tuberculosis is suspected.1
Treatment is mainly symptomatic. Xerophthalmia can be treated with artificial tears. Symptomatic xerostomia can be treated with sialogogues provided there is some residual salivary function. Sialogogues can be mechanical, such as chewing gum; gustatory, such as citric acid–containing foods or fluids or sweet-tasting substances; or pharmacologic, such as pilocarpine hydrochloride. For patients without functioning salivary gland parenchyma or whose salivary glands do not respond to stimulation by sialogogues, saliva substitutes can be prescribed.1 Effective teeth brushing with a fluoridated dentifrice and flossing after each meal help prevent further salivary or lacrimal gland involvement, autoimmune disease, and malignancy.1
REFERENCES:
1. Leung AK. Benign lymphoepithelial lesion (Mikulicz syndrome). In: National Organization for Rare Disorders. NORD Guide to Rare Disorders. Philadelphia, PA: Lippincott Williams & Wilkins; 2003:chap 1.17.
2. Leung AK, Wong AL, Robson WL, Pinto A. Benign lymphoepithelial lesion (Mikulicz’s syndrome) of the submandibular glands in a four-year-old boy. Otolaryngol Head Neck Surg. 1994;111(3 pt 1):
302-304.
3. Aleem A, Harakati MS, al-Momen A. Mikulicz syndrome. J Pak Med Assoc. 1997;47(4):126-129.
4. Mahmood K, Khan A, Malik SA, Ilyas S. Mikulicz syndrome, an uncommon entity in Pakistan.
J Coll Physicians Surg Pak. 2007;17(2):101-102.
5. Shimizu M, Moriyama M, Okamura K, et al. Sonographic diagnosis for Mikulicz disease. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2009;108(1):105-113.


