Arterial Ischemic Stroke in a 15-Year-Old
A previously healthy 15-year-old boy presented to the emergency department (ED) after collapsing and having developed right-sided weakness. He had participated in wrestling practice earlier that evening without incident. At approximately 4 am, he woke up to get a glass of water. Approximately 30 minutes later, his brother found him lying in the hallway. At that time, the boy was unable to move his right side and attempted to communicate with gestures. Prior to collapsing, the patient had experienced a severe headache.
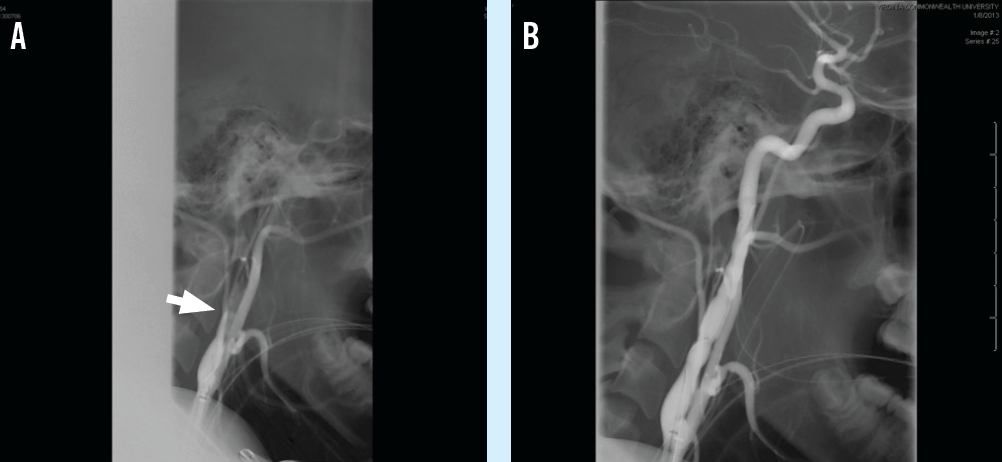
(A) A presurgical angiogram of the left common carotid artery showed tapered occlusion of the internal carotid artery (arrow).
(B) The internal carotid artery was shown on angiogram to be patent after mechanical thrombectomy.
On arrival to the ED, the patient was noted to have lethargy, right-sided facial droop, and diminished strength in his right upper and lower extremities. His pulse was 74 beats/min with a blood pressure of 133/78 mm Hg. He was given a 9-mg bolus of tissue plasminogen activator (tPA) and was started on a continuous intravenous tPA drip. A computed tomography angiogram (CTA) revealed a left internal carotid artery (ICA) dissection with occlusion. Because of concern for a hemorrhagic stroke, tPA infusion was discontinued. The patient was then transferred to a tertiary academic medical center ED.
In the tertiary ED, his vital signs were significant for a blood pressure of 135/75 mm Hg. CTA was repeated and confirmed the partial occlusion of the left ICA. The patient was taken to the operating room by neurovascular surgery for diagnostic angiography, the results of which showed tapering of the left ICA just above the bifurcation of the common carotid (A). He underwent a mechanical thrombectomy with resolution of the arterial dissection (B).
Postoperatively, he was transferred to the pediatric intensive care unit and was started on a heparin drip. During the remaining hospitalization, he was bridged from heparin to daily warfarin therapy. Findings of a medical evaluation for hypercoagulability were negative. He was evaluated by multiple services, including physical medicine and rehabilitation (PM&R), physical therapy (PT), occupational therapy (OT), and speech-language pathology (SLP). At discharge, the boy’s strength returned to baseline, but he continued to exhibit signs and symptoms of expressive aphasia. Follow-up appointments were arranged with PT, OT, SLP, and PM&R.
Arterial ischemic stroke (AIS) is uncommon among children younger than 18 years of age. The annual incidence ranges from 1.2 to 8 per 100,000 children.1 Of those cases, 3% are fatal, and more than 70% of children who sustain an AIS will have chronic disability.1
The International Pediatric Stroke Study,2 enrolling 676 children worldwide, showed that 53% of study participants who sustained AIS had arteriopathies (arterial abnormalities on vascular studies) as a risk factor. Among participants with arteriopathies, arterial dissections were the third leading cause of AIS, having occurred in 20% of that subgroup.
Arterial dissection results from the separation of the arterial layers, thus creating a false lumen. Dissections can occur as a result of trauma or may form spontaneously. Several connective tissue and vascular disorders have been associated with the formation of arterial dissections.3
Carotid dissection, although rare overall, is a frequent cause of AIS among children and adolescents. The current guidelines for management of AIS among pediatric patients (younger than 18 years of age) are based on data extrapolated from adult data. The use of intravenous thrombolytic agents such as tPA is considered experimental given the lack of clinical trials and prospective studies of its use in the pediatric population. However, results of the Thrombolysis in Pediatric Stroke (TIPS) trial,4 a 5-year prospective trial examining the use of intravenous tPA in children aged 2 to 17 years, will be crucial for creating evidence-based recommendations for treating pediatric patients with AIS.
References
1. Lyle CA, Bernard TJ, Goldenberg NA. Childhood arterial ischemic stroke: a review of etiologies, antithrombotic treatments, prognostic factors, and priorities for future research. Semin Thromb Hemost. 2011;37(7):786-793.
2. Mackay MT, Wiznitzer M, Benedict SL, Lee KJ, deVeber GA, Ganesan V; International Pediatric Stroke Study Group. Arterial ischemic stroke risk factors: the International Pediatric Stroke Study. Ann Neurol. 2011;69(1):130-140.
3. Gdynia H-J, Kühnlein P, Ludolph AC, Huber R. Connective tissue disorders in dissections of the carotid or vertebral arteries. J Clin Neurosci. 2008;15(5): 489-494.
4. Ellis MJ, Amlie-Lefond C, Orbach DB. Endovascular therapy in children with acute ischemic stroke: review and recommendations. Neurology. 2012;79(13 suppl 1):S158-S164.


