Bone Tumors of Childhood: Benign or Malignant?
Uncertainty about the significance of bony lesions found on radiographs, either incidentally or during specific investigation, can lead to confusion and anxiety. Many such lesions are benign tumors requiring minimal further evaluation or intervention, but malignant bone lesions in children can have similar presentations and similar radiographic findings.
When reviewing a bony tumor found on a radiograph, it is important to identify the age and sex of the patient, the location of the lesion (bone and the portion of that bone; epiphysis, diaphysis, or metaphysis; cortex, medulla, or surface), and the radiographic characteristics of the lesion. Tumors that are small, multiple in number, without cortical destruction, and well defined often are benign. Lesions that have indistinct margins, cortical destruction, associated periosteal reaction, large size, and soft-tissue extension are more concerning and are potentially malignant.1
Benign tumors can be categorized based on the type of material or matrix they produce: bone forming, cartilage forming, fibrous, or cystic. The 6 cases presented here are not an exhaustive list of benign bone tumors but rather are examples of common lesions encountered in children.
Case 1: Osteoid Osteoma
A 17-year-old boy presents with thigh pain that is worse at night but is relieved by ibuprofen (Figure 1).

Figure 1 — Osteoid osteoma, a benign bone-forming tumor, on the proximal right femur of a 17-year-old boy.
Osteoid osteoma is a benign, bone-forming tumor that typically presents during the second decade of life, with a 2 to 3 times higher incidence in boys. It most commonly affects the proximal femur, but other common locations include the tibia, the remainder of the femur, and the posterior elements of the spine.2 The typical presentation is a patient who has persistent, focal pain that is worse at night. Often the pain is dramatically relieved by aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs). Patients also may present with a limp, leg-length discrepancy, or scoliosis.
On radiographs, osteoid osteomas typically have a small (<1.5 cm) radiolucent nidus with an indistinct, sclerotic margin of reactive bone.3 The nidus is known to produce prostaglandins. Approximately 25% of osteoid osteomas are not obvious on plain radiographs and may require further imaging. Computed tomography (CT) or magnetic resonance imaging (MRI) may be useful in clarifying the diagnosis if the plain radiographs are not diagnostic.
Treatment is based on the severity of symptoms. Osteoid osteomas can be managed with observation and anti-inflammatory medications, and they may regress spontaneously within 2 to 3 years. If the symptoms or prolonged NSAID use are not tolerable, definitive treatment involves surgical excision or percutaneous radiofrequency ablation.
Case 2: OSTEOCHONDROMA
A 16-year-old boy presents with a palpable mass just proximal to the left knee that is painful after minimal trauma (Figure 2).

Figure 2 — Osteochondroma, a benign, cartilage-forming tumor, on the distal left femur of a 16-year-old boy.
Osteochondroma is a benign, cartilage-forming tumor that typically presents during the second decade of life, affecting boys more commonly than girls. The most common location is the distal femur, followed by the proximal tibia, proximal femur, and humerus.4 Osteochondromas typically present as painful masses associated with local trauma. They also can cause mechanical irritation, functional problems, deformity, and pathologic fractures.
An osteochondroma is a cartilage cap on a sessile or pedunculated bony base. On radiographs, they appear as bony spurs protruding from the cortex of the bone. Plain radiographs usually are diagnostic. Osteochondromas typically are located at the metaphysis and grow away from the joint. Growth ceases at puberty with physeal closure. There is a less than a 1% risk of malignant transformation to chondrosarcoma with solitary osteochondromas.1 Multiple hereditary exostoses (also known as hereditary multiple osteochondromas) result from an autosomal dominant condition characterized by 2 or more exostoses in the appendicular and axial skeleton. This condition carries an increased risk of malignant transformation ranging from 1% to 20%. MRI is useful for evaluating the cartilage cap if concern exists for possible malignant transformation.
Treatment of osteochondromas typically is conservative, but surgical excision may be considered if patients have significant pain, mechanical symptoms, cosmetic concerns, or malignant transformation.
Case 3: FIBROUS DYSPLASIA
An 18-year-old young woman with a history of precocious puberty and unilateral café au lait macules presents with right hip pain (Figure 3).
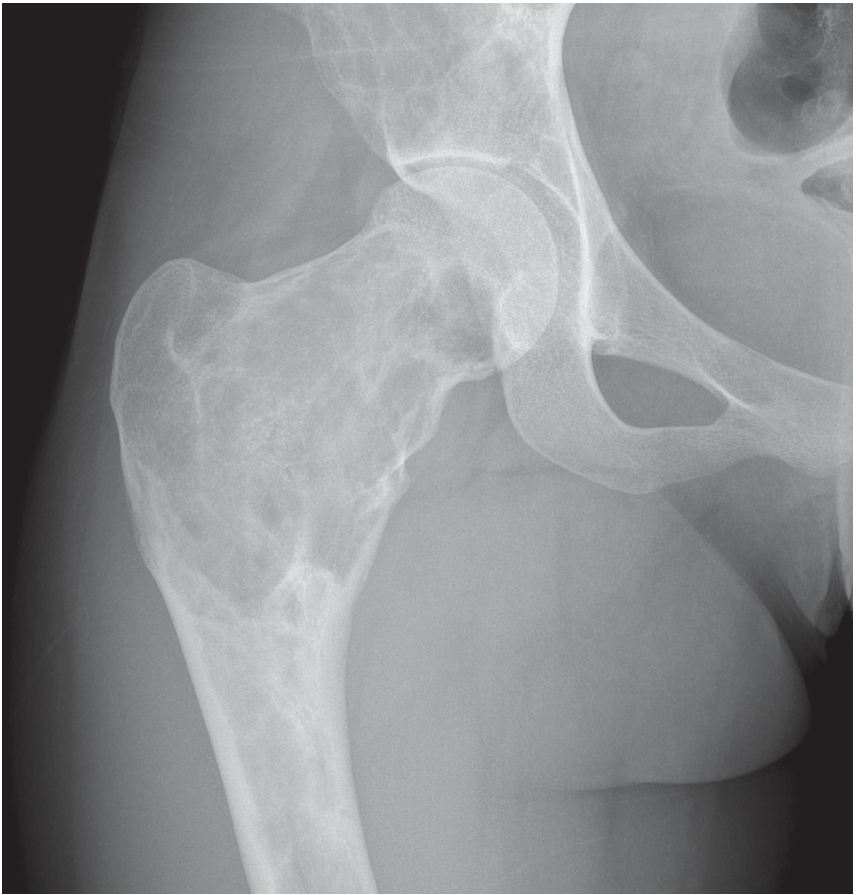
Figure 3 — Benign fibrous dysplasia of the right proximal femur and pelvic bone in an 18-year-old young woman.
Fibrous dysplasia is a benign fibrous tumor that typically presents during adolescence, affecting boys and girls equally. Fibrous dysplasia is monostotic in approximately 80% of cases and polyostotic in the other 20%. Polyostotic fibrous dysplasia is seen in McCune-Albright syndrome, which is a triad of precocious puberty, café au lait spots, and polyostotic fibrous dysplasia. The most common locations for monostotic fibrous dysplasia, in descending order of frequency, are the ribs, proximal femur, tibia, and skull. These lesions typically are asymptomatic but may have associated pain, swelling, pathologic fracture, or bone deformity.4,5
On radiographs, fibrous dysplasia appears as a lucent, homogenous, ground-glass opacity in the diaphysis or metaphysis, often expanding and deforming the bone. The cortical bone typically is scalloped without any periosteal reaction. Plain radiographs usually are diagnostic, but CT may be useful in evaluating the spine, pelvis, chest, or facial bones.
Treatment varies with the size and symptoms of the lesion. If the integrity of the bone is stable, then observation is often adequate. Bisphosphonates have been used in the treatment of adults and may have a role in the treatment of severely affected children. Treatment with curettage and bone grafting often is unsuccessful. Orthopedic surgical intervention may be necessary if there is impending or associated pathologic fracture.
Case 4: NONOSSIFYING FIBROMA
A 9-year-old girl presents with superficial abrasions and knee pain following an automobile accident (Figure 4).

Figure 4 — A nonossifying fibroma, a benign fibrous tumor, in the distal femur of a 9-year-old girl.
Nonossifying fibromas (NOFs), also known as fibrous cortical defects (FCDs), are benign, fibrous tumors that affect boys and girls equally. While the terms often are used interchangeably, NOF refers to lesions larger than 3 cm, and FCD refers to lesions smaller than 3 cm. NOFs are the most common benign bone lesion of childhood, occurring in as many as 35% of children. They most commonly occur in the distal femur and the proximal or distal tibia. They usually are solitary and asymptomatic and often are discovered as an incidental radiographic finding. However, larger lesions occupying more than 50% of the diameter of the bone can be associated with pathologic fracture.4
On radiographs, NOFs typically are metaphyseal, eccentric, lucent lesions with scalloped, well-marginated, sclerotic borders and no cortical or periosteal reaction. Plain radiographs usually are diagnostic. Treatment for classic lesions is observation, since they usually regress during late adolescence.
Case 5: UNICAMERAL BONE CYST
A 16-year-old female volleyball player presents with left shoulder pain (Figure 5).
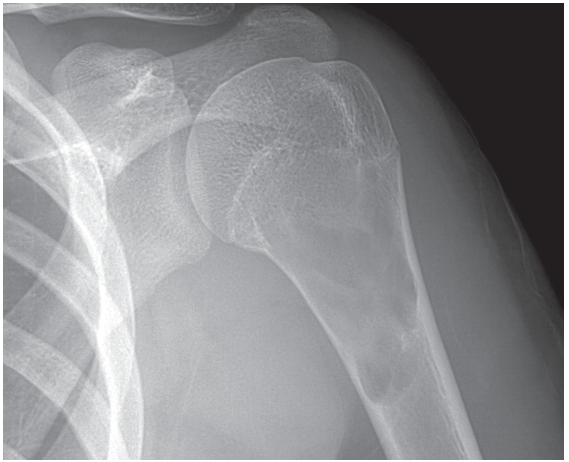
Figure 5 — A benign unicameral bone cyst in the proximal humerus of a 16-year-old girl.
A unicameral bone cyst (UBC) is a cystic tumor that is fluid-filled with a thin fibrous lining. It generally occurs in the first 20 years of life and has a 2:1 male to female ratio. It most commonly affects the proximal humerus and femur. UBCs usually are asymptomatic and often do not present until pathologic fracture occurs or are discovered incidentally.1
On radiographs UBCs are central, metaphyseal, lytic lesions with well-defined, thin, sclerotic margins that involve nearly the entire diameter of the bone and may slightly expand the cortex. Pathologic fracture of UBCs may have the fallen fragment sign, where a fragment of cortical bone falls to the base of the cyst.6 Plain radiographs usually are diagnostic, and axial imaging is helpful only if the lesion is located in the pelvis.
Among the treatment options for bone cysts are observation, corticosteroid injection, and bone grafting or other surgical procedures. Closed treatment of pathologic fractures is possible and frequently results in resolution of the lesion. Otherwise, these lesions in most cases will resolve spontaneously by adulthood.
Case 6: ANEURYSMAL BONE CYST
An 11-year-old girl presents with right knee pain following a low-impact injury while playing soccer and is unable to bear weight (Figure 6).

Figure 6 — An aneurysmal bone cyst on the right proximal tibia of an 11-year-old girl.
Aneurysmal bone cysts (ABCs) are benign, vascular tumors that grow rapidly and destroy bone. They typically are solitary lesions of adolescence that affect girls slightly more often than boys. They most commonly are located in the metaphyseal area of long bones but also are found in the posterior spinal elements and can be found in any bone in the body. They typically present with pain and pathologic fracture; neurologic deficit is possible if the spine is involved.
The typical radiographic appearance of an ABC is an aggressive, well-circumscribed, expansile, eccentric, lytic lesion. They are described as having a soap-bubble appearance. Plain radiographs may be diagnostic, but if there is any uncertainty or if the lesion is not in a long bone, axial imaging can clarify the diagnosis by demonstrating multiple fluid–fluid levels in the cystic spaces.1
Surgical treatment of ABCs usually is required and consists of curettage and bone grafting with or without internal stabilization, depending on the size and location of the lesion. A significant risk of recurrence exists in up to 20% these lesions after treatment.
REFERENCES:
1. Yildiz C, Erler K, Atesalp AS, Basbozkurt M. Benign bone tumors in children. Curr Opin Pediatr. 2003;15(1):58-67.
2. Orlowski JP, Mercer RD. Osteoid osteoma in children and young adults. Pediatrics. 1977;59(4):
526-532.
3. Springfield DS, Gebhardt MC. Bone and soft tissue tumors. In: Morrissy RT, Weinstein SL, eds.
Lovell & Winter’s Pediatric Orthopaedics. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006:493-550.
4. Copley L, Dormans JP. Benign pediatric bone tumors: evaluation and treatment. Pediatr Clin North Am. 1996;43(4):949-966.
5. Biermann JS. Common benign lesions of bone in children and adolescents. J Pediatr Orthop. 2002;22(2):268-273.
6. Reynolds J. The “fallen fragment sign” in the diagnosis of unicameral bone cysts. Radiology. 1969;92(5):949-953.


