Until very recently, when it came to chronic cough, children were to be treated like little adults. In its 1998 guidelines on cough, the American College of Chest Physicians (ACCP) stated that "the approach to managing chronic cough in children is similar to the approach in adults."1
Newly published guidelines from the ACCP take an entirely different view.2 Those guidelines mandate a management approach for children younger than 15 years that is clearly distinct from that for adults. In fact, an entire 23-page article is devoted to the elaboration of the management principles and strategy that are uniquely appropriate for children. What follows here is a summary of the key amendments reflected in these new guidelines.
BASIC PRINCIPLES
A first and fundamental difference between the new pediatric and adult guidelines is the definition of chronic cough: in children, this is "a daily cough that lasts longer than 4 weeks" (vs 8 weeks in adults). This time frame is based on a review of the natural history of upper respiratory tract infections in children.
The touchstone of effective management is that treatment should be directed toward the cause of chronic cough. With few exceptions, empiric and symptomatic treatment are strongly discouraged.
EVALUATION
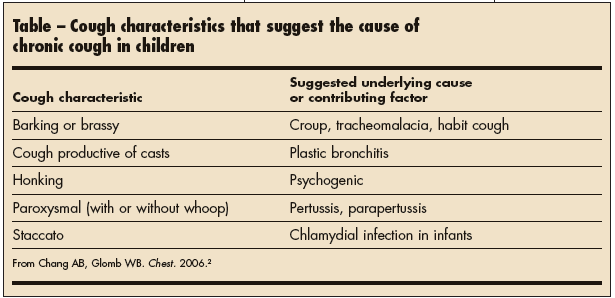
Any child with chronic cough needs to be carefully evaluated for symptoms and signs of a systemic or underlying respiratory disease. Sometimes—unlike in adults—specific characteristics of the cough can themselves suggest the diagnosis (Table). Other clinical findings can also offer diagnostic clues.
The guidelines recommend that any evaluation of chronic cough in a pediatric patient include, at a minimum, chest films and spirometry (if age-appropriate). Chronic productive purulent cough is always pathologic, and its evaluation usually includes a number of specialized investigations.
Many suspected causes are actually rare. The guidelines summarize the available evidence on a number of clinical entities that have sometimes been cited as causes of isolated cough in children. These include:
• Upper airway cough syndrome (formerly called postnasal drip syndrome).
• Gastroesophageal reflux disease (GERD).
• Atopy.
• Arnold ear-cough reflex.
• Environmental pollutants.
• Pertussis and other respiratory infections.
• Foreign-body aspiration.
• Airway lesions.
• Asthma.
All of these entities—even asthma—are, in fact, uncommon causes of isolated cough in children. However, they should not be entirely excluded from the differential diagnosis. This caveat applies in particular to pertussis and foreign-body aspiration, both of which can have serious consequences yet are easily missed.
Two rare causes of cough you don't want to miss. Although pertussis, parapertussis, and Mycoplasma infections typically cause cough with a distinctive pattern or in association with other symptoms, chronic cough may be their sole manifestation. This is especially likely in children who have been vaccinated against pertussis or who have recently received antibiotic therapy. Suspect pertussis in children with persistent cough—even if they are fully immunized—if they have had known contact with a person with pertussis infection.
Because a foreign body lodged in the airway for any length of time can result in long-term pulmonary damage, take pains not to miss this diagnosis. Children who have inhaled a foreign body usually present acutely. However, chronic cough can be the presenting symptom if the diagnosis was missed. Keep in mind that normal findings on a chest radiograph do not rule out foreign-body inhalation.
If evaluation of a child with chronic cough reveals an underlying cause, the cough is said to be specific. Treatment is then directed toward the underlying disease process. However, if no clues to a possible cause are identified, the cough is nonspecific.
TREATMENT OF NONSPECIFIC COUGH
The new guidelines caution strongly against the empiric treatment of nonspecific chronic cough in children. Dr Anne Chang, lead author on the pediatric guidelines, explains why: it has been well documented that there are 3 main causes of chronic cough in adults (asthma, GERD, and upper airway cough syndrome), and this knowledge is the basis for rational empiric treatment in that setting. However, there are few data on the most common causes of chronic cough in children—and the information that does exist suggests that the most common causes in adults account for less than 10% of chronic cough in children. Moreover, as Dr Chang points out, some of the agents included in the adult protocol for empiric treatment (eg, sedating, or first-generation antihistamines) can have serious adverse effects in children. Thus, the adult protocol for empiric treatment of chronic cough is clearly inappropriate for children.

Watch, wait, reevaluate. The recommended strategy is watchful waiting, followed by reevaluation for the emergence of specific etiologic signs if the cough persists. Most nonspecific chronic cough in children is thought to be post-viral or the result of another nonserious process and will resolve spontaneously.
Empiric treatment for suspected asthma-related cough. There is a single exception to contraindicated empiric therapy. A course of low-dose inhaled corticosteroids (400 µg/d equivalent of budesonide( or beclomethasone) may be tried in a child with chronic nonspecific cough who has risk factors for asthma. However, the trial regimen should last no longer than 2 or 3 weeks. If the cough has not resolved by that time, the medication should be stopped rather than the dosage increased.
Dr Chang notes that it is not uncommon to see children who have been given steadily increased dosages of corticosteroids--sometimes for months or even years--for a cough that turned out not to be asthma-induced. She hopes the new guidelines will help prevent such situations. "There's no doubt that children with asthma can present with cough," she says. "The key is that if you treat a child for asthma-related cough, the cough should go away within 2 to 3 weeks. If it doesn't, you need to consider another diagnosis." Even better, she points out, is to diagnose asthma before starting treatment.
The disappearance of cough after a trial of corticosteroids does not necessarily mean that the patient has asthma. The cough may have resolved spontaneously. Further evaluation is needed to establish the diagnosis.
In those rare instances in which other medications may be prescribed as empiric treatment for nonspecific cough, a similar approach is recommended: the trial should be no longer than the expected response time, and if the cough does not resolve within that time, the drug should be withdrawn and other diagnoses considered.
Symptomatic therapy strongly discouraged. There is no evidence that agents of any class are effective for symptomatic relief of nonspecific cough in children, and many drugs used for this purpose are potentially harmful.
• Antibiotics—there is some evidence of benefit in children in whom there is reason to believe sinusitis is the cause of cough or in whom the cough has become wet or moist but in no other setting.
• ß2-Agonists—no evidence supports their use in children with chronic cough.
• Anticholinergic agents—there is no evidence to support their use for nonspecific cough in children.
• Antihistamines—evidence of their efficacy for relieving acute cough in children is minimal at best; they are unlikely to be effective against chronic cough. Dr Chang points out that antihistamines can have a number of adverse effects in children, including sedation, breathing depression, excitability, and complications of excitability (eg, injuries from running or jumping).
• Central-acting antitussives (eg, codeine, dextromethorphan()—these are expressly contraindicated in children, especially young children, notes Dr Chang, because of their potential to cause breathing difficulties or respiratory arrest.
The guidelines recommend that no over-the-counter (OTC) cough or cold medications be used. The ingredients such medications contain are combinations of the ineffective and sometimes dangerous ingredients listed above. In addition, these drugs—which tend to taste good and look pretty—are frequently ingested unintentionally by young children. Dr Chang adds that overdosing, sometimes to the point of incidental poisoning, is also a common problem with OTC cough medications. In part, this results from confusing dosing information on the packages, but it is also because the basic ineffectiveness of these preparations leads parents to keep giving more.
Working effectively with parents. Parents are understandably anxious about their child's cough and may expect their health care provider to prescribe or recommend medication. The new guidelines acknowledge the importance of addressing parents' fears and expectations. They recommend taking the time to explain to parents the typical course of respiratory infections in children and the ineffectiveness of medications for nonspecific cough. This can help allay fears and demands for drugs.
For parents who feel compelled to do something specific for their child, Dr Chang suggests such relatively harmless nonpharmacologic remedies as menthol( rubs or honey and lemon (in children who can eat sugar). Menthol has shown some ability to reduce cough sensitivity in laboratory studies, and sugar-and-lemon drinks can help soothe the throat. She discourages the use of steam for children, citing cases in which patients have been accidentally burned.
Finally, the new guidelines recommend working with parents to eliminate environmental factors that can exacerbate cough. Most often, this means suggesting interventions to help parents stop smoking. However, other measures can sometimes help: for example, keeping the house warmer at night may help reduce nocturnal coughing in children in whom asthma is suspected as the cause of the cough.


