Chronic Exertional Compartment Syndrome: Myths, Misconceptions, and Fallacies
ABSTRACT: Chronic exertional compartment syndrome (CECS) is a frequently overlooked and disregarded activity-related condition. Primary care practitioners are often the first healthcare providers to see patients with symptoms of the challenging-to-diagnose CECS. This article discusses 10 of the most common myths, misconceptions, and fallacies surrounding the condition.
Chronic exertional compartment syndrome (CECS) is one of the most overlooked diagnoses in clinical and sports medicine. Its onset is typically insidious and has a variety of different presentations. CECS can easily be confused with other conditions. Because CECS is usually self-remitting with the discontinuation of the inciting activity, it can easily be disregarded by the patient and/or overlooked by the physician.
Primary care practitioners are often the initial healthcare provider to evaluate a patient’s presenting symptoms. It is important to be familiar with CECS, so as to know when a referral to a sports medicine specialist, orthopedist, and/or podiatrist for undiagnosed, unmanageable pain is needed.
In my personal practice, I have evaluated over 100 patients referred for suspected CECS. This article addresses 10 of the myths, misconceptions, and fallacies regarding this condition, patient complaints, pathophysiology, evaluation, management, outcomes, and recurrence perspectives.
CECS must be differentiated from delayed-onset muscle soreness syndrome (DOMS).
In both conditions, pain is the predominant symptom. In DOMS, however, pain and muscle stiffness are associated with vigorous exercise or work-related activity and are noted after the activity is completed. They typically occur at the start of training during the sport activity or the work effort. Over a few days with rest, the symptoms resolve spontaneously. With conditioning and unlike CECS, DOMS symptoms no longer occur even with the continuation of the activity, as the person with DOMS gets more “in shape.” DOMS is common in athletes starting vigorous training programs in preparation for their season’s sport.
Myth 1: CECS is a well-defined, easily recognized condition.
Although much is written about CECS, none of the descriptions seems to completely address the variety of presentations and degrees of symptoms that can be associated with it.1 Customarily, CECS is defined as pain in the legs associated with activity, but it may also include numbness, paresthesia, and muscle weakness secondary to muscle swelling within an individual’s myofascial compartments. Furthermore, it is not limited to legs, as CECS has been reported in the thighs, gluteal muscles, upper extremities, and feet. Symptoms usually resolve after the patient ceases the activity.
CECS should be considered in the differential diagnosis of any patient who presents with recurrent pain or any of the other aforementioned symptoms with high repetition activities, such as running, dancing, walking, gymnastics, and weight lifting. The skeletal muscle of the anterior compartment of the leg is the most frequent site affected in patients with CECS.
Because of the vagueness of CECS symptoms and their resolution upon stopping the activity, the patient and the physician often attribute the symptoms to overuse or muscle fatigue. Physicians may tell the patient to try cross-training with a different exercise or activity instead of continuing the inciting activity. This recommendation is largely why CECS is one of the most missed diagnoses in clinical medicine.
What’s the “Take-Away”?
The reproducible nature of its symptoms with activity and the resolution of symptoms with cessation of the activity are the essential components of making a CECS diagnosis.
Myth 2: The pathophysiology of CECS is definitively established.
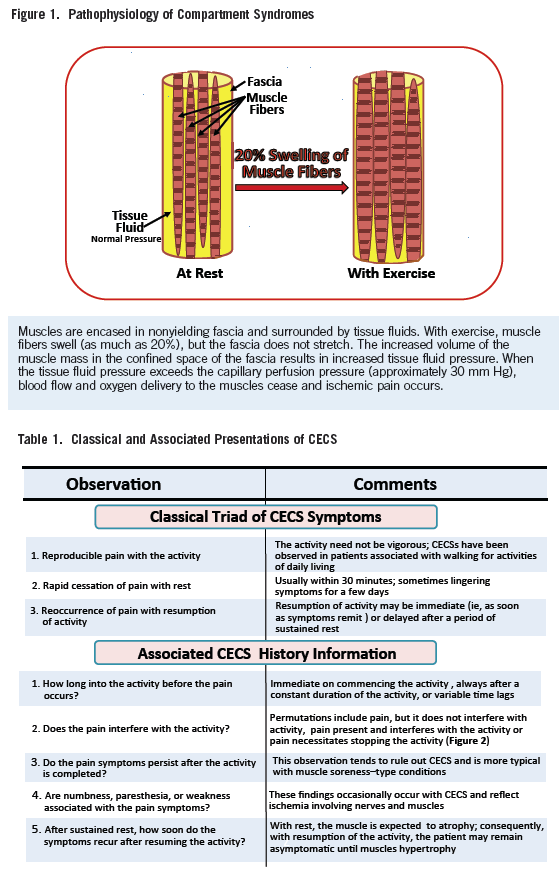
The consensus is that exercise increases muscle swelling and the swelling is restricted by the confines of the fascia surrounding the muscle (Figure 1).2 This swelling increases the intracompartmental pressure because the fascial boundary is relatively nonyielding. The muscles become ischemic and the symptoms are manifested as pain when the compartment pressure exceeds the capillary perfusion pressure.3
This explanation seems entirely adequate for the acute skeletal muscle compartment syndrome (SMCS). However, when applying this description to the pathophysiology of CECS, there are several unresolved issues:
•Why does pain typically remit immediately after the cessation of the activity in patients with CECS while it persists in patients with acute SMCS, despite the fact that swelling and ischemia appear to be the predominant pathology in both conditions?
• Why are many lower-extremity presentations unilateral in patients with CECS even though both lower extremities would be expected to have similar levels of exertion, swelling, and degrees of ischemia?
• Why do symptoms immediately recur in patients with CECS, after a sustained period of rest and expected muscle atrophy, when the activity inciting the condition is again resumed?
• Why is CECS not more often observed in body builders and weight lifters whose muscle compartments are hypertrophied to enormous proportions and whose training includes repetitive motion exercises?
• Why do patients with CECS typically remain pain free when at rest with relatively high muscle compartment pressures (>15 mm Hg), whereas pain is typically present at these pressure levels in patients with acute SMCS?
• Why do patients with CECS not always have relief of symptoms after fasciotomies?
• Why does CECS almost never develop into an acute SMCS with continuation of the activity—which may be possible perhaps due to endorphins and/or overriding the pain symptoms with strong motivation to complete the activity?
What’s the “Take-Away”?
While the pathophysiology of CECS and SMCS appear to have similar features, acute SMCS has highly reproducible features that are well explained by the proposed pathophysiology. CECS, with many unanswered questions and presenting variations, warrants the label of a syndrome. Regardless, the patient’s history is the
essential feature in evaluation, treatment, and management.
Myth 3: Pain with activity is the only essential feature of CECS history.
While pain with activity is typically the “driving force” that leads the patient to seek medical evaluation, other considerations to fully appreciate his or her pain report must be considered (Table 1).These include the time of pain onset (eg, at the start of activity, after a usually highly reproducible time into the activity and variable time lag.
The primary care practitioner should always ask the following questions when evaluating a patient with suspected CECS:
• Does the pain merely interfere with the activity or does it cause the patient to cease performing the activity?
• Do the pain symptoms worsen, remain the same, or improve with the continuation of the activity and/or with training and possibly physical therapy.
• Does the pain remit quickly (ie, within 15 to 30 minutes) after stopping the activity or does it persist?
• Is numbness distal to the muscle compartment, weakness of the muscle groups, or paresthesia associated with the pain symptoms?
• Finally, does it take days or weeks before the pain symptoms recur after a sustained period of rest?
What’s the “Take-Away”?
The classic triad presentation of CECS is that of (1) pain that is usually highly reproducible and occurs after a finite period of time into the activity, (2) pain severe enough to interfere or halt the activity, and (3) rapid cessation of pain with stopping the activity. Most patients, however, do not present with this classical triad of findings. Consequently, further information from the examination and muscle compartment pressure measurements is needed to confirm the diagnosis and make appropriate treatment recommendations.
A fraction of an inch discrepancy in limb length or joint range of motion from a deformity can have an enormous additive effect with a highly repetitive activity, such as running. For example, if the deformity results in the overwork of the involved compartment muscles by 1/16 of an inch with each loading (ie, the stance phase of the gait cycle), approximately 2000 repetitions (assuming a 2.5-ft stride) will occur to run a mile. The involved muscle will have to do a summated 125 in (2000 x 1/16 in) of extra excursion activity. When multiplied by a runner who weighs 170 lb, this computes to 2125 ft-lb of extra work. Hence, small deformities and/or asymmetries can summate to enormous amounts of overuse and help to explain quantitatively why the patient was prone to develop CECS.

Myth 4: Few useful findings can be found in the asymptomatic patient who is being evaluated for CECS during the time of the examination.
While pain with activity is the symptom that leads the patient to seek medical attention, information from the examination can help support or rule out CECS. There are 12 components of the examination that should be addressed with each CECS evaluation (Table 2).3 Even a minor discrepancy or asymmetry can overwork the muscle activity of a compartment, cause the muscle to hypertrophy, and initiate the unilateral presentation of CECS.
Some frequently observed findings on the examination of a patient with CECS include exceptionally well-developed musculature and a feeling of muscle fascia tautness of the involved compartment when pressing on the area. Pain localization is also important. If the pain occurs when symptomatic in a joint, in or on the bone, or is worsened with joint motions, a CECS diagnosis is unlikely. Tenderness of the involved muscle compartment is almost never observed, again attesting to the importance of patient history. Finally, the findings of muscle atrophy and/or peripheral neuropathy are not consistent with CECS.
A particularly useful component of the examination for CECS is the single stance provocative stress test, which is used to accentuate the muscle masses of the anterior and posterior compartments. It is executed by single stance standing—first in as much equinus as possible, followed by in as much ankle dorsiflexion as possible. Rock hard, bulging muscles are consistent, but not necessarily the sole criterion, for a diagnosis of CECS of the respective compartments.
What’s the “Take-Away”?
While there may be a dearth of physical examination findings with CECS, the presence or absence of certain findings can help to confirm the CECS diagnosis. Of particular importance are the development of the musculature of the compartment and the recognition of any deformity that leads to overuse stresses of the muscles in the compartment.

Myth 5: Compartment pressure measurements (manometrics) are essential for confirming the CECS diagnosis.
Although manometrics are used as the “gold standard” in making a CECS diagnosis, their interpretations raise questions. In the asymptomatic patient at rest, a compartment tissue fluid pressure of 15 mm Hg or higher is used as the criterion for a CECS diagnosis, especially if it is supported by the patient’s history and the examination is consistent with CECS.4
The muscle compartment pressure measurements must be interpreted in light of the patient’s symptoms at the time the measurements are taken (see Myth 6). It seems counterintuitive that an absolute measurement confirms the presence of a CECS, whereas the published reports demonstrate a wide variation of pressures that dictate a fasciotomy be performed for acute SMCS (Table 3).5-11 I recommend using a pain grading system that makes the diagnosis of CECS an art rather than just a science (see Myth 6, Figure 2).
What’s the “Take-Away”?
Manometrics are useful in confirming the CECS diagnosis, but additional information is essential before making a recommendation for fasciotomy.

Two systems are predominantly used for measuring tissue fluid pressures. The first and least expensive is the Whitesides technique.5 With the Whitesides technique, a fluid column is connected to a 3-way stopcock with 1 limb connected to an 18-gauge intravenous needle that is inserted into the muscle compartment, the second limb to a blood pressure manometer, and the third limb to a fluid-filled syringe. Fluid in the syringe is used to pressurize the system. The first movement of the fluid meniscus in the tubing connected to the muscle compartment indicates that the fluid pressure in the compartment has been exceeded. The reading on the blood pressure manometer indicates the fluid pressure in the compartment.
The second method is use of an electronic pressure monitor. In this system, an 18-gauge needle with a small vent hole just proximal to the bevel at the end of the needle is connected to the electronic monitor and the reservoir that interphases with the needle and the monitor is filled with saline. The monitor is “zeroed” at the level of the compartment, and the needle is inserted into the muscle compartment. Approximately 0.1 cc of fluid is then injected into the muscle. A direct pressure reading in mm Hg is displayed on the monitor.
Another technique for measuring skeletal muscle compartment pressures is the use of a pressure transducer, such as that used for arterial lines and central venous pressures. By connecting the fluid-filled transducer tubing to an 18-gauge needle and inserting the needle into the muscle compartment, a tissue pressure measurement can be obtained. This is a quick and relatively easy technique to use in the operating room, where this equipment is usually available from the anesthesiologist.
Myth 6: The interpretation of compartment pressures for making a CECS diagnosis is absolute.
As mentioned, the diagnosis and, even more importantly, the recommendation to have a fasciotomy must be interpreted in light of the patient’s pain symptoms.12 To make this objective on one hand and an art on another, I instruct my patients to grade their pain on a 0 to 10 point scale (0=no pain, 10=excruciating pain requiring narcotic analgesics). The patient is asked to grade his or her pain on a variety of permutations, such as: pain level at the time of this examination, worst pain level ever experienced, and pain level 30 minutes after discontinuing the exercise. This information helps with the interpretation of the severity of the symptoms and provides the criteria of whether to add a stress (ie, exercise) component to the CECS evaluation (Figure 3).
For example, if a patient presents with a pain level of 0 at the time of the examination and while at rest (on the 0-10 scale), and the compartment pressures is ≥15 mm Hg, I am comfortable recommending a fasciotomy if he or she wants to continue the activity that precipitates the symptoms.
Conversely, if a patient’s pain level is 5 at rest and the compartment pressures are normal, the symptoms are probably due to something other than CECS.
A third permutation might be when compartment pressures approach 15 mm Hg and the patient has a level 3 or 4 pain at rest. In this situation, an exercise challenge and immediate repeat compartment pressure measurements are indicated. Two limbs of the algorithm arise from this permutation. If the pain symptoms increase and the pressures are >20 mm Hg criterion, a fasciotomy is recommended. If pain symptoms remain unchanged with repeat testing—ie, pain symptoms do not increase with the exercise—repeat pressure testing is deferred (see Myth 7, Figure 3).
What’s the “Take-Away”?
The integration of the patient’s pain symptoms with the compartment pressure measurements and the addition of an exercise challenge add further objectivity to the recommendations of whether a fasciotomy would benefit the patient.

Myth 7: A standard exercise test should be performed whenever the exercise challenge of the chronic exertional algorithm is needed.
Although the majority of patients experience their symptoms while engaged in running activities, other common stressors include walking (especially in nonathletic older patients), dancing, stair climbing, and prolonged standing. When an exercise challenge is needed for the CECS evaluation, personalize the challenge with an action that is analogous to the activity that precipitates the patient’s symptoms.
The time it takes to develop the symptoms and the level of exertion (whether maximal, marked, moderate, or minimal)—confirmed with pulse and blood pressure measurements immediately upon completion of the exercise challenge)—are recorded. More importantly, have the patient prescribe a level of pain (on the 0-10 point scale) to the exercise challenge.
If no pain occurs with the challenge, repeat post-exercise pressure testing is deferred (Figure 3). In some cases, patients have rested from the activity long enough so that their muscles atrophy and symptoms do not recur until an exercise program is resumed and their involved muscles hypertrophy. If this is the situation, and if the patient so desires, advise him or her to resume the exercise activity/training program until pain symptoms are noted, then return and do a pain-producing exercise challenge that generates the same symptoms. Immediately repeat muscle compartment pressure measurements thereafter.
What’s the “Take-Away”?
Use your patient’s history and pain symptom severity to select an analogous exercise challenge. When equivocal compartment pressure measurements are obtained at rest, the exercise challenge is indicated. If the symptoms do not recur with the exercise challenge, post-exercise pressure measurements should be deferred and the patient should be given the option to resume the exercise activity until symptoms recur with it, and then return for the repeat exercise challenge.
Myth 8:It is necessary to measure the pressures in all compartments when performing pressure testing for CECS.
Theoretically, the patient with reports of CECS in both legs could have 16 compartment measurements—4 leg muscle-facial compartments in each leg, while at rest and after exercise testing—with an 18-gauge needle. I feel, however, that this is unwarranted, and unnecessarily painful for the patient, even when local anesthetic is used to numb the skin at the needle entry sites. This is where the patient history is so crucial.
First, the history helps localize the compartments where the symptoms occur so that measurements can be limited to only those target areas. Second, if the symptoms are bilateral, it is unnecessary to study the pressures in both legs. Rather, the compartment pressures from the pressure-measured leg can be reasonably assumed to be similar in the opposite limb that has equally symptomatic muscle compartments. Third, if the resting pressures paired with the patient’s pain symptoms (on the 0-10 scale) are high enough (see Myth 6, Figure 3), an exercise test and post-exercise measurements are unnecessary. With this approach, 16 possible pressure measurements can be reduced to a single compartment pressure measure.
However, if the major symptoms are confined to a single compartment, but the patient experiences symptoms to a lesser degree in other compartments with his or her exercise activity, I recommend that pressures in these compartments be measured. If sufficiently elevated, fasciotomies should also be done for them. This recommendation is based on my observation that, after a single compartment fasciotomy, the lesser symptomatic compartments can develop CECS symptoms when the patient resumes exercise activities. Often, the patient returns for a reevaluation and additional pressure measurements of what was the lesser symptomatic compartment at the initial study.
What’s the “Take-AWAY”?
With a comprehensive history and use of the symptom grading scale, needle sticks with the large bore testing equipment can be kept to a minimum. It is also appropriate to generalize that the same problem is occurring in the opposite limb when symptoms are bilateral, obviating the need for bilateral limb compartment pressure measurements. Finally, symptoms that occur to a lesser degree in a muscle compartment should have manometrics done with exercise testing (if needed for confirmation) and fasciotomies (if indicated by the muscle pressure testing) as they may become the limiting factors upon resumption of full activities.
Myth 9: Once a fasciotomy is performed for CECS, the patient’s CECS symptoms are always relieved.
With the anterior compartment fasciotomy, there is a 80% to 100% likelihood of returning to the activity level that was possible before the CECS patient became symptomatic.1,13-15 With other compartment fasciotomies, there is a 50% to 65% likelihood of full,
asymptomatic activity.
Even with fasciotomies, there is a small possibility that the symptoms will reoccur, anywhere between 6 months to 20 years. When this occurs and is confirmed by the history, examination, and manometrics, the patient should be given the option of repeat surgery versus stopping the inciting activity and replacing it with alternative exercises. The repeat surgery should consist of repeat fasciotomies and, if the fascia is scarified, fasciectomies.
What’s the “Take-AWAY”?
Share outcome expectations with the patient—that symptoms can recur after a period of recovery, be it months to years, and that the fascia may have reconstituted itself and/or may have been replaced with scar tissue. In these situations, a reevaluation followed by exploration, repeat fasciotomy, or a complete removal of the fascia may be needed if the patient wants to continue the exercise activity.
Myth 10: Because surgery is usually the recommendation for confirmed CECS, the primary care practitioner has a minimal role in managing a patient with this problem.
The primary care practitioner is likely the first healthcare provider to diagnose and treat a patient who may present with CECS. The condition should be considered in the differential diagnosis of any patient who presents with leg or muscle location pain (whether or not it is associated with exercise). This is especially true when the cause of a pain—eg, stress fracture, muscle strain, claudication, neuropathy, or periostitis (shin splints)—are not consistent with the history and examination. If the CECS is suspected, timely referral for muscle compartment pressure testing will obviate the need for expensive testing interventions (eg, MRI, nuclear medicine scans, single-photon emission CT, muscle biopsies, and electromyography).
Note: There are now fellowships in sports medicine for primary care practitioners, and an awareness of CECS is important fundamental knowledge for this subspecialty.
What’s the “Take-AWAY”?
There is no better caregiver for initial recognition of CECS than the primary care practitioner. The history and examination are the primary information sources for making the CECS diagnosis. From this information, recommendations for muscle compartment pressure testing and/or surgery (ie, fasciotomy) can be made confidently.
As our population becomes more exercise-minded, the number of patients dealing with CECS will likely increase. The primary care practitioner remains on the frontline, seeing patients who complain of a variety of different symptoms that can be indicative of CECS. When CECS is suspected, the patient’s history and examination should be evaluated to determine if the symptoms are strongly supportive of the CECS diagnosis, consistent with this diagnosis, or do not support a CECS diagnosis.
When history and examination findings are strongly supportive or consistent with the CECS diagnosis, the patient should be scheduled for compartment pressure measurements. The interpretation of the pressure measurements using the 3 aforementioned perspectives, coupled with the history and examination, provides the necessary information to decide whether or not to recommend a fasciotomy.
Finally, the primary care practitioner’s recognition of CECS can help create a logical management plan for the patient—whether it be cross training with a different activity or surgery. Although the incidence of CECS is relatively low, recurrent muscle-related pain associated with a defined activity that is not responsive to rest, physical therapy, and/or the use of NSAIDs, should always raise an “index of suspicion” that the cause is CECS.
Acknowledgment: Phi-Nga Jeannie Le, MD, Houston, TX, assisted with the editing and content of this manuscript.
Michael B. Strauss, MD, is an orthopaedic surgeon who focuses on managing limb-threatening wounds, medical director of hyperbaric medicine at Long Beach Memorial Medical Center, a clinical professor of orthopaedic surgery at the University of California Irvine, and orthopaedic consultant for the Foot & Ankle Clinic at the Veterans Affairs Medical Center in Long Beach, CA.
References:
1. Fraipont MJ, Adamson GJ. Chronic exertional compartment syndrome. J Am Acad Orthop Surgeons. 2003;11(4):268-276.
2. Fronek J, Mubarak SJ, Hargens AR, et al. Management of chronic exertional anterior compartment syndrome of the lower extremity. Clin Orthop Relat Res. 1987;220:217-227.
3. Styf JR, Körner LM. Microcapillary infusion technique for measurement of intramuscular pressure during exercise. Clin Orthop Relat Res. 1986;207:253-262.
4. Pedowitz RA, Hargens AR, Mubarak SJ, Gershuni DH. Modified criteria for objective diagnosis of chronic compartment syndrome in the leg. Am J Sports Med. 1990;18(1):35-40.
5. Whitesides TE, Haney TC, Morimoto K, Harada H. Tissue pressure measurements as a determinant for the need of fasciotomy. Clin Orthop Relat Res. 1975;113:43-51.
6. Sheridan GW, Matsen FA 3rd. Fasciotomy in the treatment of the acute compartment syndrome. J Bone Joint Surg Am. 1976;
58(1):112-115.
7. Murbarak SJ, Owen CA, Hargens AR, et al. Acute compartment syndromes diagnosis and treatment with the aid of the wick catheter. J Bone Joint Surg Am. 1978;60(8):1091-1095.
8. Matsen FA 3rd, Winquist RA, Krugmire RB Jr. Diagnosis and management of compartmental syndromes. J Bone Joint Surg Am. 1980;62(2):286-291.
9. Heckman MM, Whitesides TE, Grewe SR, et al. Histological determination of the ischemic threshold in the canine compartment syndrome model. J Orthop Trauma. 1993;7(3):199-210.
10. Matava MJ, Whitesides TE Jr, Seiler JG 3rd, et al. Determination of the compartment pressure of muscle ischemia in a canine model. J Trauma. 1994;37(1):50-58.
11. McQueen MM, Court-Brown CM. Compartment monitoring in tibial fractures, the pressure threshold for decompression. J Bone Joint Surg Br. 1996;78(1):99-104.
12. Strauss MB, Wakim N. Patient perception pinpoints exertional leg pain. BioMechanics. 2002;9(10):63-77.
13. Rorabeck CH, Fowler PJ, Nott L. The results of fasciotomy in the management of chronic exertional compartment syndrome. Am J Sports Med. 1988;16(3):224-227.
14.Styf JR, Korner LM. Chronic anterior compartment syndrome of the leg: results of treatment by fasciotomy. J Bone Joint Surg Am. 1986;68(9):1338-1347.
15.Howard JL, Mohtadi NG, Wiley JP. Evaluation of outcomes in patients following surgical treatment of chronic exertional compartment syndrome in the leg. Clin J Sport Med. 200;10(3):176-184.


