Is Fever Good or Bad? Helping Parents Understand the Difference
ABSTRACT: Fever is a consequence of an immune process that is initiated internally by an infection or endogenous process such as a collagen vascular disease. Understanding the aspects and historical nature of the fever can help in determining a process for intervention. Utilizing criteria may be helpful for infants, but most decisions are based on the clinical likelihood of bacterial disease versus viral disease. Addressing “fever phobia” in caregivers and school personnel may be the most difficult hurdle, but it should be discussed early during well-child visits.
Fever is one of the main reasons children are brought to clinics and emergency departments. Misconceptions about fevers in children have persisted for decades among caregivers and health care workers alike. In 1980, Schmitt coined the term fever phobia to refer to the unrealistic concerns about fever and its harmful consequences in children.1 Schmitt found that 52% of parents bringing their children to a hospital-based pediatric clinic believed that a moderate fever of 40°C (104°F) or less could cause serious neurologic consequences.1
Twenty years later, Crocetti et al2 found that fever phobia still persisted: 21% of parents with children enrolled in 1 of 2 hospital-based pediatric clinics thought brain damage was the primary harmful effect of fever, and 14% listed death as a harmful effect. Parents also stated that they would check their febrile child’s temperature once or more per hour and would awaken the child to give antipyretics. Crocetti et al also found that parents gave antipyretics for normal temperatures (< 37.8°C [100°F]) and at incorrect dosing intervals, placing the children at increased risk of toxicity.
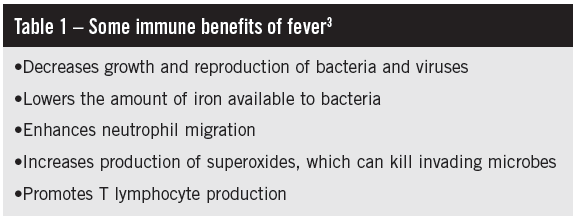
Many parents and caregivers incorrectly believe that fever itself is an illness that can be “cured” with antipyretics, not a result of an insult to the body. Misconceptions about fever exist across all ethnicities, education levels, and genders.1,2 The role of the medical professional is to explain the causes, usefulness (Table 1), and consequences of fever to caregivers.
PATHOPHYSIOLOGY OF FEVER
Fever is a consequence of the inflammatory response system reacting to a perturbation of the body’s homeostasis (ie, viral or bacterial infection). When such insult occurs to the body, macrophages release cytokines including interleukin-1, interleukin-6, and tumor necrosis factor. These cytokines function as endogenous pyrogens, increasing the level of prostaglandin E2 produced by the anterior hypothalamus. The anterior hypothalamus is the body’s temperature regulator, and prostaglandin E2 acts to increase the body’s set point. When the body’s thermostat elevates initially, several mechanisms respond to help raise the internal temperature, thus producing a fever. The concert of mechanisms includes skeletal muscle shivering, increased cellular metabolism, minimization of heat loss through vasoconstriction at the skin, and decreased sweating.3
TAKING A FEVER HISTORY
Knowing that a child has a fever is only part of the story. It is important to know more about the history of present illness before acting on a fever alone. During history taking, ask about other symptoms, including but not limited to how the child is acting and eating/drinking and whether upper or lower respiratory symptoms or gastrointestinal symptoms are present. Further questioning narrows the differential diagnosis and focuses on the possible cause of fever.
Take, for example, 2 children with a temperature of 39°C (102.2°F). The first child appears well, with clear rhinorrhea and no other findings on examination; the second child is hard to awaken for examination and has low blood pressure. For the first child, a practitioner likely would feel comfortable with a diagnosis of upper respiratory infection, likely viral in origin, requiring symptomatic care and no antibiotics. The second child likely is more ill, could be septic or have meningitis, and thus would require further workup and, possibly, antibiotics. Both children presented with the same elevation in temperature; however, each patient’s history changed the clinical decision-making process.
FEVER EVALUATION
Several criteria4,5 are used to help evaluate a fever in an otherwise well-appearing infant with a normal physical examination (Table 2). Infants who meet these criteria are considered as being at low risk for serious bacterial infection and can be monitored closely without antibiotics.
CASE 1: FEVER WITH INFECTION
A 6-week-old infant presents with upper respiratory symptoms and wheeze. The infant is noted to be febrile, with a temperature of 38.5°C (101.3°F), respiration rate of 40 breaths per minute, oxygen saturation of 97% on room air, and in no respiratory distress. During the initial evaluation, testing for respiratory syncytial virus (RSV) is positive.
Symptomatic care for RSV without further significant investigation for another infection is appropriate in an otherwise healthy appearing infant less than 8 weeks old.6-8 Symptomatic care includes nasal cannula if oxygen saturation is low, nasal saline with suctioning, chest physiotherapy, and albuterol if effective. Titus and Wright6 found that the risk of serious bacterial infection is remote in an infant younger than 8 weeks with RSV infection, especially compared with febrile infants without RSV infection. The authors note that there is still a clinically relevant rate of urinary tract infections and therefore recommend obtaining urine cultures. Liebelt et al7 studied infants 90 days and younger with similar results: The risk of bacteremia, urinary tract infection, and meningitis were very low in infants with RSV. Kuppermann et al8 found that no patient younger than 2 years with RSV had bacteremia, whereas 2.7% of their patients younger than 2 years without RSV had bacteremia.
In review, the current recommendations for an otherwise healthy-appearing 6-week-old infant with RSV is to obtain a urine culture and to treat symptomatically for RSV. Blood cultures and spinal fluid analysis can be withheld as long as the infant appears well.
CASE 2: FEVER WITHOUT A SOURCE
A 2-year-old girl presents with a 2-day history of fever. The highest temperature noted by her mother has been 39.6°C (103.2°F). Aside from the fever, the patient has no other symptoms or complaints. On examination, the patient appears well and has no focal findings suggesting a source for the fever. At the time of examination, the patient is noted to have a temperature of 38.9°C (102.1°F).
The diagnosis of a fever without a source is a common one, especially among this age group. Given that an acute viral illness is the most likely cause of fever in a patient of this age with benign findings on physical examination, evaluation and management should be focused on ruling out a treatable cause. With no other signs or symptoms present, it is prudent to perform a urinalysis and a urine culture (best obtained via catheterization or suprapubic aspiration vs bag collection) to rule out underlying urinary tract infection.9 Additional workup is not warranted unless the child developed additional symptoms or signs suggesting focal infection or a worsening underlying disease.
Management of this patient is guided by physical examination and laboratory test findings. In the absence of a treatable source of infection, symptomatic management and close follow-up are warranted. However, if physical examination or laboratory test findings (eg, positive urinalysis) suggest a treatable source of infection, appropriate empirical antibiotic therapy should be initiated while awaiting the results of culture tests.
CASE 3: FEBRILE SEIZURE
A 4-year-old boy is presented by his mother after having had an episode of whole-body “shaking.” The mother reports that before this episode, the child had been irritable and that he had “felt warm” upon awakening that morning, with a fever of 38.6°C (101.5°F). A few minutes after waking, he had a “shaking episode,” which episode lasted a few minutes and resolved spontaneously. The week prior to this episode, the patient had developed upper respiratory tract symptoms, which have been improving. The patient’s father and older brother have a history of similar episodes occurring when they were younger; the episodes had resolved as they grew older. At the time of examination, the patient is awake, alert, and afebrile. Physical examination reveals right acute otitis media.
The diagnosis of a simple febrile seizure is made clinically. Typically occurring in children between 6 months and 5 years of age, simple febrile seizure is a generalized seizure that lasts less than 15 minutes and is associated with a fever. Patients experiencing simple febrile seizures should have a complete return to baseline mental status following the episode, and they typically have only 1 seizure in a 24-hour period. A family history of febrile seizures is common.
Further evaluation and workup is warranted for patients with persistent seizures, a failure to return to baseline mental status, or signs and symptoms suggesting intracranial infection. Computed tomography, magnetic resonance imaging, and electroencephalography are not indicated for a simple febrile seizure in a child who has completely recovered from the episode and has a normal physical examination.10 Children younger than 6 months and those with signs and symptoms suggesting intracranial infection are no longer considered to have simple febrile seizure but are classified as having a complex febrile seizure. These children require lumbar puncture, a basic metabolic panel, a complete blood count, and assessment of magnesium, phosphorus, and glucose levels to identify any metabolic or infectious cause for the seizure.
Two things must be done when caring for patients with simple febrile seizures. The first (and arguably most difficult) is educating the parents about the condition. The second is identifying and treating the source of the patient’s fever. Little can be done to prevent recurrent simple febrile seizures. Antipyretics do not prevent recurrent febrile seizures, and continuous or intermittent anticonvulsant medications are not recommended for the prevention of simple febrile seizures.10,11

CASE 4: PNEUMONIA
An 8-year-old girl is brought by her parents for a fever associated with 1 week of cough and congestion that has worsened despite supportive care and now is associated with new abdominal pain. On physical examination, the patient is found to be febrile (38.9°C [102°F]) and slightly tachypneic but otherwise well appearing. Crackles are noted at the base of the left lung.
The patient’s history and physical examination are sufficient to make the diagnosis of pneumonia and begin appropriate antibiotic therapy. Pneumonia is an infection of the lung parenchyma that is either viral (eg, RSV, influenza, parainfluenza, adenovirus) or bacterial (eg, Streptococcus pneumoniae, Haemophilus influenzae, Mycoplasma pneumoniae) in nature. The infection is often characterized by fever, cough, and tachypnea with crackles, egophony, bronchophony, or whispered pectoriloquy noted on examination. Dyspnea, chest or abdominal pain, malaise, hypoxia, nasal flaring, grunting, and retractions also may be present.
Chest radiography can help support the diagnosis but likely will not change the management. However, if physical findings suggest pleural effusion, chest radiography would be warranted to assess the extent of pleural disease and help further guide management. Note that if the patient continues to be ill despite therapy, a chest radiograph can be obtained to assess for new-onset pleural effusion or to assess the extent of pulmonic involvement.12
Inpatient versus outpatient management depends on the clinical appearance of the patient and the presence or absence of hypoxia and extent of respiratory distress. In this case, the progression of upper respiratory symptoms to persistent fever, mild respiratory distress, and new-onset abdominal pain suggests a viral process that has progressed to bacterial pneumonia. In this patient’s age group, the most likely pathogen is S pneumonia. Treatment with high-dose amoxicillin should be sufficient.12
Close follow-up is warranted to assess for worsening respiratory status or disease progression despite antibiotic therapy. Failure to improve within 48 to 72 hours warrants further evaluation; a chest radiograph can be obtained to assess for pleural effusion and the extent of pulmonic involvement. The presence of extensive pulmonic disease or pleural effusion likely will require further inpatient management with intravenous antibiotics and/or chest tube placement and drainage of the pleural effusion.12 Changes in management and further evaluation always depend on the patient’s clinical presentation; therefore, patients warrant close follow-up after treatment has been initiated.
CASE 5: FEVER OF UNKNOWN ORIGIN
A 15-year-old boy is brought by his parents for evaluation of persistent fever of 38.9°C (102°F) for more than 2 weeks. He denies any other symptoms and appears well. The patient has a benign physical examination and no other complaints.
The diagnosis of a fever of unknown origin is difficult. The definition of fever of unknown origin varies and can be defined as any of the following13:
•An illness with a temperature of 38.4°C (101.1°F) or higher at least 10 of the previous 14 days without a cause determined via history, physical examination, or laboratory screening.
•A minimum of 2 weeks of daily temperature above 38.2°C (100.8°F) with no cause despite laboratory tests and physical examination.
•Fever for 8 days or longer with no determined cause.
The top causes of a fever of unknown origin are infection (30% to 35%), collagen vascular disease (20%), and malignancy (10%). Approximately 30% of cases likely will resolve without ever having a diagnosis.13
When evaluating a patient with a fever of unknown origin, an extensive and thorough history and physical examination must be performed. During initial assessment, it is important to determine the onset and height of fever, the method in which the temperature has been taken, and the presence or absence of constitutional symptoms such as weight loss, night sweats, chills, and anorexia. An extensive history that addresses travel; sexual activity; animal exposure or tick bites; tuberculosis exposure; history of blood transfusion; recent trauma, fracture, or puncture wounds; history of heart disease; immune deficiency; foreign body ingestion; presence of a central venous line; current medications; immunizations; and allergies will help identify potential sources for the fever and help focus the evaluation. An extensive physical examination should be performed to identify any potential source that could be contributing to the persistence of the patient’s fever.
Initial laboratory workup should include complete blood count, comprehensive metabolic panel, C-reactive protein, erythrocyte sedimentation rate, blood culture, urinalysis, and urine culture. Serology testing for HIV, Epstein-Barr virus, and cytomegalovirus and tuberculin skin testing should be strongly considered. Chest radiography to evaluate for underlying subclinical pulmonary disease also can be performed. In the well appearing patient, initial evaluation should be done as an outpatient. The patient should be followed up closely for new symptoms or changes in physical examination suggestive of a source for the fever. Long-term management is driven by the patient’s clinical appearance and the results of the initial laboratory testing. A rheumatology or infectious disease should be considered to guide evaluation and management.13
WHEN TO TREAT A FEVER
It is important to educate the family that fever itself is not a danger, and that it actually may benefit the child. Since fever itself is not a threat, administering antipyretics simply because the child is febrile is not recommended. Antipyretics are useful to improve the comfort of a febrile child. The improved comfort of the child could be due to normalization of temperature and/or the analgesic effect of the antipyretic, but the exact mechanism is unknown.14
The most commonly used and approved medications in children are acetaminophen and ibuprofen. It is important to counsel the caregiver about the appropriate dosage and timing interval of these medications to avoid overdosing. Combination therapy, alternating acetaminophen and ibuprofen, can be confusing to caregivers and can lead to incorrect dosing and therefore overdosing. Because of the risk of confusion and overdose, and the lack of evidence that combination therapy is faster or more effective, it is recommended that caregivers use one antipyretic.15
Acetaminophen generally is given as 10 to 15 mg/kg/dose and can be dosed every 4 to 6 hours but should not exceed 4 doses in 24 hours. Ibuprofen generally is given at 10 mg/kg/dose and can be dosed every 6 to 8 hours but no more than 3 times in 24 hours. Most infant acetaminophen formulations no longer come in the 80 mg/0.8 mL solution, since this was confusing to parents. The common dosing for children and infants for acetaminophen is 160 mg/5 mL and for ibuprofen is 100 mg/5 mL.
REFERENCES:
1. Schmitt BD. Fever phobia: misconceptions of parents about fevers. Am J Dis Child. 1980;134(2):
176-181.
2. Crocetti M, Moghbeli N, Serwint J. Fever phobia revisited: have parental misconceptions about fever changed in 20 years? Pediatrics. 2001;107(6):1241-1246.
3. Sullivan JE, Farrar HC; Section on Clinical Pharmacology and Therapeutics, Committee on Drugs. Fever and antipyretic use in children. Pediatrics. 2011;127(3):580-587.
4. Jaskiewicz JA, McCarthy CA, Richardson AC, et al; Febrile Infant Collaborative Study Group. Febrile infants at low risk for serious bacterial infection—an appraisal of the Rochester criteria and implications for management. Pediatrics. 1994;94(3):390-396.
5. Baker MD, Bell LM, Avner JR. The efficacy of routine outpatient management without antibiotics of fever in selected infants. Pediatrics. 1999;103(3):627-631.
6. Titus MO, Wright SW. Prevalence of serious bacterial infections in febrile infants with respiratory syncytial virus infection. Pediatrics. 2003;112(2):282-284.
7. Liebelt EL, Qi K, Harvey K. Diagnostic testing for serious bacterial infections in infants aged 90 days or younger with bronchiolitis. Arch Pediatr Adolesc Med. 1999;153(5):525-530.
8. Kuppermann N, Bank DE, Walton EA, Senac MO Jr, McCaslin I. Risks for bacteremia and urinary tract infections in young febrile children with bronchiolitis. Arch Pediatr Adolesc Med. 1997;
151(12):1207-1214.
9. Finnell SM, Carroll AE, Downs SM; Subcommittee on Urinary Tract Infection. Technical report—
diagnosis and management of an initial UTI in febrile infants and young children. Pediatrics. 2011;128(3):e749-e770.
10. Oluwabusi T, Sood SK. Update on the management of simple febrile seizures: emphasis on minimal intervention. Curr Opin Pediatr. 2012;24(2):259-265.
11. Steering Committee on Quality Improvement and Management, Subcommittee on Febrile Seizures American Academy of Pediatrics. Febrile seizures: clinical practice guideline for the long-term management of the child with simple febrile seizures. Pediatrics. 2008;121(6):1281-1286.
12. Bradley JS, Byington CL, Shah SS, et al; Pediatric Infectious Diseases Society, Infectious Diseases Society of America. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25-e76.
13. Tolan RW Jr. Fever of unknown origin: a diagnostic approach to this vexing problem. Clin Pediatr (Phila). 2010;49(3):207-213.
14. Mayoral CE, Marino RV, Rosenfeld W, Greensher J. Alternating antipyretics: is this an alternative? Pediatrics. 2000;105(5):1009-1012.
15. Adam HM. Physiology and management of fever. In: McInerny TK, Adam HM, Campbell DE, Kamat DM, Kelleher KJ, eds. Textbook of Pediatric Care. Elk Grove Village, IL: American Academy of Pediatrics; 2009;418-422.


