ABSTRACT: There are 2 principal types of benign vascular tumors—hemangiomas—commonly seen in infants. Infantile hemangiomas, which are the most common, usually appear 2 to 3 weeks after birth, grow rapidly over the next 6 months, then begin to involute. Most infantile hemangiomas involute completely by the time a child is 9 or 10 years old. Congenital hemangiomas, as their name implies, are present and fully developed at birth. Some congenital hemangiomas involute rapidly over the first year of life; other congenital hemangiomas are noninvoluting.
 Infantile hemangiomas are benign vascular tumors that are not usually present at the time of birth but instead typically become evident within the first 2 to 3 weeks of life. They are the most common benign tumor of infancy, characterized by a period of rapid growth followed by gradual involution.1 Congenital hemangiomas are vascular tumors that are fully formed at birth and that do not exhibit accelerated postnatal growth. Some congenital hemangiomas involute rapidly over the first year of life, while others persist indefinitely without treatment.
Infantile hemangiomas are benign vascular tumors that are not usually present at the time of birth but instead typically become evident within the first 2 to 3 weeks of life. They are the most common benign tumor of infancy, characterized by a period of rapid growth followed by gradual involution.1 Congenital hemangiomas are vascular tumors that are fully formed at birth and that do not exhibit accelerated postnatal growth. Some congenital hemangiomas involute rapidly over the first year of life, while others persist indefinitely without treatment.

Figure 2 – The subcutaneous nodule/tumor on this infant's fourth finger, the overlying skin of which has a blue hue, is an example of the deep type of infantile hemangioma.
It is important for pediatricians to be able to distinguish between the various types of hemangiomas that are seen in infants. Such knowledge is key to providing proper, accurate anticipatory guidance to families regarding their infants' vascular lesions.
INFANTILE HEMANGIOMAS
Although infantile hemangiomas may occur anywhere on the body, they are seen most often in the head and neck regions. Infantile hemangiomas may present with a variety of precursor lesions, and in up to 50% of affected infants, these preceding cutaneous marks are evident at birth. Precursor lesions include areas of telangiectases, erythematous macules, or even bruising. Most infantile hemangiomas begin their growth phase in the first few weeks of life, although deeper subcutaneous hemangiomas are occasionally not noticed until patients are a few months old.2

Figure 3 – The infantile hemangioma seen here is a mixed, or combined, type; it demonstrates a melding of the patterns seen in
Figures 1 and
2.
Clinical findings. The appearance of infantile hemangiomas varies depending on the location of the tumor within the skin; they may occur as superficial, deep, or mixed lesions. Superficial hemangiomas are bright red to scarlet-colored lobulated papules, plaques, or nodules (Figure 1). Deep hemangiomas usually present as subcutaneous nodules, often with an overlying blue hue and visible surface telangiectases (Figure 2). Combined hemangiomas have both a superficial and a deep component (Figure 3).3 In the majority of uncomplicated cases, the clinical impression suffices for diagnosis.
Infantile hemangiomas express and stain positively for glucose transporter 1 (GLUT-1), a marker that is also found in placental tissue. This fact has fascinated researchers; some hypothesize that infantile hemangiomas may form when placental progenitor cells break off early in utero and form independent lesions in the skin.

Figure 4 – The infantile hemangioma seen here is in the process of involuting. Note the gray center, which represents the area where the vessels have begun their regression.
Growth phase. A natural history of growth followed by eventual, spontaneous involution is characteristic of infantile hemangiomas. In the majority of these lesions, the most rapid growth usually occurs in the first 6 months. Most infantile hemangiomas have reached their maximum size by the time patients are 9 to 12 months old, although this often occurs earlier with lesions that are small and localized. Nonetheless, the growth characteristics of any given infantile hemangioma can be difficult to predict, and it is important to explain this fully to parents. Complications are possible, especially in the setting of higher-risk lesions, such as those near the eye (which may interfere with the proper development of the visual axis) and those that surround the airway (the rapid growth of which can cause stridor and necessitate emergency medical management).2
nvolution phase. In superficial infantile hemangiomas, the onset of the involution phase is marked by a color change from bright red to dull red, purple, or gray (Figure 4). This process typically begins centrally and then spreads to the periphery of the lesion over time. Deeper lesions tend to become smaller, more compressible, and less blue. It is estimated that complete involution of infantile hemangioimas occurs at a rate of 10% per year, such that 50% have 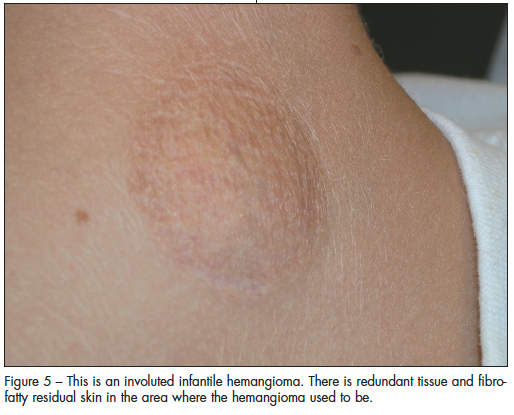 involuted by the time patients are 5 years of age, 70% by 7 years of age, and 90% by 9 to 10 years of age. However, involution is not always associated with the return of completely normal skin. Possible residual changes after involution include telangiectases, atrophy, scarring, and redundant skin (Figure 5).2
involuted by the time patients are 5 years of age, 70% by 7 years of age, and 90% by 9 to 10 years of age. However, involution is not always associated with the return of completely normal skin. Possible residual changes after involution include telangiectases, atrophy, scarring, and redundant skin (Figure 5).2
Management. The majority of infantile hemangiomas are localized and pose no immediate or lasting threat; for these lesions, observation and routine monitoring by a pediatrician or dermatologist are acceptable treatment options. A minority of infantile hemangiomas can cause significant morbidity, however, and these require early recognition, timely referral to a specialist, and prompt intervention and therapy to minimize complications.
Worrisome presentations include multiple cutaneous hemangiomas and location in any of the following regions: periocular; periorificial; nasal tip; large segmental facial; neck, lower lip, chin, and mandibular areas (beard distribution); and lumbosacral spine.3 Treatment decisions and options for these clinical variants can be challenging and may require a multispecialist approach. Discussion of these higher-risk lesions is beyond the scope of this article, but an understanding of which lesions require referral is of paramount importance; timely referral is essential in order not to miss the window of opportunity that will allow treatment to minimize morbidity or cosmetic deficits.
For optimal long-term cosmetic outcome, pediatric plastic surgery is sometimes helpful in the case of infantile hemangiomas that involute but leave behind fibrofatty residua.
CONGENITAL HEMANGIOMAS

Figure 7 – This bright red–violaceous plaque is a rapidly involuting congenital hemangioma (RICH) in an early stage.
Congenital hemangiomas are less common than infantile hemangiomas. There are 2 major types: the rapidly involuting congenital hemangioma (RICH) and the noninvoluting congenital hemangioma (NICH).4,5 Both RICH and NICH are usually solitary and are most commonly found on the head or on the limbs, near a joint.4
Clinical findings. Because they are fully developed at the time of birth, congenital hemangiomas are often observed in utero via antenatal ultrasonography. They demonstrate high-flow output on duplex Doppler examination.
At birth, NICH presents as a round to ovoid tumor that is violaceous and that has overlying tiny or coarse telangiectases, often with a surrounding pale halo (Figure 6). The presentation of RICH may be similar to that of NICH, or RICH may resemble a typical infantile hemangioma in appearance (Figure 7). Both RICH and NICH have an average diameter of several centimeters.4
RICH and NICH express different vascular markers from those in classic infantile hemangiomas. Instead of GLUT-1, congenital hemangiomas express markers that indicate higher vascular flow. Although certain academic centers now have the ability to stain biopsy tissue for these markers, it has not become common practice to biopsy hemangiomas for this purpose, since in most uncomplicated cases, the clinical impression is sufficient for diagnosis. In patients in whom RICH or NICH is suspected but in whom the diagnosis cannot be confirmed clinically, ultrasonography can be a helpful study. Ultrasonographic documentation of higher flow patterns suggests the diagnosis of congenital hemangioma. In patients who are doing poorly clinically or who require definitive or aggressive medical management, a biopsy specimen of the hemangioma can be sent for special staining and a precise diagnosis.

Figure 8 – This rapidly involuting congenital hemangioma is in a later stage (the child is almost 1 year old); it shows a classic pattern of atrophy left in the wake of rapid resolution.
Natural history. Although RICH and NICH may have a similar clinical appearance, they have dissimilar natural histories. Clinical follow-up is the key to distinguishing between the 2 types of congenital hemangioma, because their behavior is very different within the first year of life.
RICH undergoes rapid involution early in life, with postnatal regression usually starting soon after birth; typically, regression is complete by the time a patient is 14 months old. RICH often results in a residual patch of thin skin with prominent veins and diminished subcutaneous tissue but normal blood flow (Figure 8). NICH, on the other hand, typically persists unchanged or with slight expansion and remains a fast-flow lesion on duplex Doppler examination.6 Both the rapid involution of RICH and the persistence of NICH may possibly be explained by the higher vascular flow of these lesions.
In some patients, RICH has been associated with the development of heart failure from cardiac overload as well as with decreased platelet counts; both comorbidities are thought to result from localized intravascular coagulation.7
Management. Observation remains the standard of care for uncomplicated cases of RICH and NICH. In cases of hemodynamic instability, cardiology consultation is warranted. Surgery can often correct any postinvolution redundancy or potential bleeding.5
Plastic surgery may provide improved outcomes in children with a RICH lesion that results in cutaneous atrophy after involution and in those with NICH in whom telangiectases persist for years beyond infancy.





 Infantile hemangiomas are benign vascular tumors that are not usually present at the time of birth but instead typically become evident within the first 2 to 3 weeks of life. They are the most common benign tumor of infancy, characterized by a period of rapid growth followed by gradual involution.1 Congenital hemangiomas are vascular tumors that are fully formed at birth and that do not exhibit accelerated postnatal growth. Some congenital hemangiomas involute rapidly over the first year of life, while others persist indefinitely without treatment.
Infantile hemangiomas are benign vascular tumors that are not usually present at the time of birth but instead typically become evident within the first 2 to 3 weeks of life. They are the most common benign tumor of infancy, characterized by a period of rapid growth followed by gradual involution.1 Congenital hemangiomas are vascular tumors that are fully formed at birth and that do not exhibit accelerated postnatal growth. Some congenital hemangiomas involute rapidly over the first year of life, while others persist indefinitely without treatment.


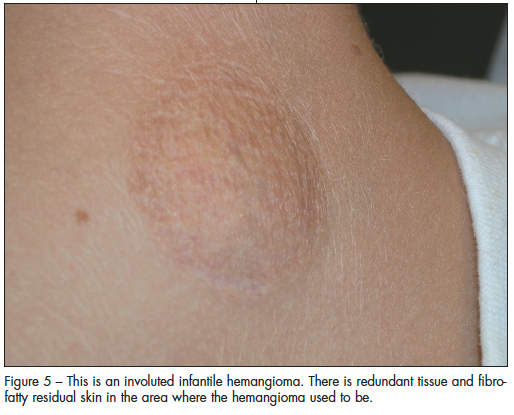 involuted by the time patients are 5 years of age, 70% by 7 years of age, and 90% by 9 to 10 years of age. However, involution is not always associated with the return of completely normal skin. Possible residual changes after involution include telangiectases, atrophy, scarring, and redundant skin (Figure 5).2
involuted by the time patients are 5 years of age, 70% by 7 years of age, and 90% by 9 to 10 years of age. However, involution is not always associated with the return of completely normal skin. Possible residual changes after involution include telangiectases, atrophy, scarring, and redundant skin (Figure 5).2

