Hemophagocytic Syndrome Caused by Mycoplasma pneumoniae
An 8-year-old boy with no significant medical history presented to the emergency department with a 12-day history of nocturnal fevers as high as 39°C. He reported 2 episodes of vomiting, fatigue, anorexia, and mild congestion in the days leading up to admission. Review of systems was otherwise normal.
Physical examination findings were unremarkable except for a 1-cm, nontender, mobile right cervical node without liver or spleen enlargement.
 Laboratory test results were significant for a normal hematocrit of 34%, a low platelet count of 136 × 103/µL, and a low white blood cell count of 2,780/µL, with 52% neutrophils, 39% lymphocytes, 2% monocytes, 2% eosinophils, and 6 atypical lymphocytes per high-power field. The erythrocyte sedimentation rate was elevated at 31 mm/h, and the C-reactive protein level was within normal limits. Aspartate aminotransferase and alanine aminotransferase were elevated at 185 U/L and 259 U/L, respectively, with normal bilirubin levels. Lactate dehydrogenase was elevated at 1,080 U/L.
Laboratory test results were significant for a normal hematocrit of 34%, a low platelet count of 136 × 103/µL, and a low white blood cell count of 2,780/µL, with 52% neutrophils, 39% lymphocytes, 2% monocytes, 2% eosinophils, and 6 atypical lymphocytes per high-power field. The erythrocyte sedimentation rate was elevated at 31 mm/h, and the C-reactive protein level was within normal limits. Aspartate aminotransferase and alanine aminotransferase were elevated at 185 U/L and 259 U/L, respectively, with normal bilirubin levels. Lactate dehydrogenase was elevated at 1,080 U/L.


Findings of urinalysis, chest radiography, and abdominal ultrasonography were all unremarkable. Blood cultures were negative for bacteria and fungi.
 On hospital day 5 (fever day 17), the patient developed an edematous, erythematous, blanching, pruritic, bright red maculopapular rash that began on his cheeks and then spread downward from head to toe over the course of 3 days.
On hospital day 5 (fever day 17), the patient developed an edematous, erythematous, blanching, pruritic, bright red maculopapular rash that began on his cheeks and then spread downward from head to toe over the course of 3 days.
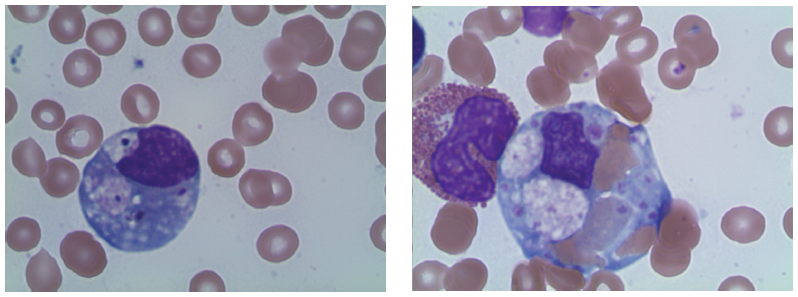
On testing, the boy’s ferritin level was found to be elevated at 2,618 ng/mL. Results of a bone marrow biopsy revealed mild hemophagocytosis (see biopsy slides). A diagnosis of infection-related hemophagocytic lymphohistiocytosis (HLH), or hemophagocytic syndrome, was tentatively made when Mycoplasma pneumoniae immunoglobulin M testing was positive on day 8 of the boy’s hospitalization.
HLH is defined according to the HLH-2004 protocol by the following 8 criteria, 5 of which must be fulfilled1:
• Fever greater than 38°C for more than 7 days
• Splenomegaly
• Bicytopenia
• Hypertriglyceridemia or hypofibrinogenemia
• Tissue demonstration of hemophagocytosis (eg, bone marrow, liver, spleen)
• Low natural killer–cell activity
• Ferritin greater than 500 ng/mL
• Soluble CD25 antigen (soluble interleukin-2 receptor) greater than 2,400 U/mL.
Standard treatment, according to this protocol, involves dexamethasone, cyclosporine A, etoposide, and intrathecal methotrexate. If these therapies fail, hematopoietic stem-cell transplantation is recommended.
 Given prior reports of M pneumoniae–associated HLH being successfully treated with less-intensive therapies without relapse,2 our patient was given a trial treatment of azithromycin for 5 days and methylprednisone (2 mg/kg/d) for 7 days. His fever improved and his rash diminished. His pancytopenia gradually resolved, and his other elevated laboratory values trended downward. One week after discharge, tests showed decreased natural killer–cell function at 9% at 50:1 dilution, confirming the diagnosis of HLH.
Given prior reports of M pneumoniae–associated HLH being successfully treated with less-intensive therapies without relapse,2 our patient was given a trial treatment of azithromycin for 5 days and methylprednisone (2 mg/kg/d) for 7 days. His fever improved and his rash diminished. His pancytopenia gradually resolved, and his other elevated laboratory values trended downward. One week after discharge, tests showed decreased natural killer–cell function at 9% at 50:1 dilution, confirming the diagnosis of HLH.
After discharge, the patient was weaned gradually off of prednisone, and he has not had a recurrence of his illness. We report this case to emphasize the importance of considering HLH in the differential diagnosis of children presenting with fever of unknown origin, and of considering M pneumoniae as a possible infectious cause that might remit with milder therapies.
 References:
References:
1. Henter JI, Horne A, Aricó M, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48(2):124-131.
2. Yoshiyama M, Kounami S, Nakayama K, Aoyagi N, Yoshikawa N. Clinical assessment of Mycoplasma pneumoniae-associated hemophagocytic lymphohistiocytosis. Pediatr Int. 2008;50(4):432-435.
Dr Cohen is a pediatrics resident at Massachusetts General Hospital for Children in Boston. Dr Chew is a neurology resident at Harvard Medical School in Boston. Dr Bourgeois is a pediatrician in the Department of Pediatrics at Boston Children’s Hospital and the Department of Pediatrics at Harvard Medical School. Dr Wolf is a pediatrician in the Department of Pediatrics at Boston Children’s Hospital.


