Her medical history was unremarkable except for normal childhood illnesses. She was allergic to cefaclor. Results of a review of systems were otherwise benign; she had no fever or malaise, no rashes, no joint swelling, and no lymphadenopathy. She denied any recent upper respiratory tract infections or other illnesses.
She walked with a very mildly antalgic gait, but her rotational profile was symmetrical and her legs were equal in length; she displayed no Trendelenburg sign. Her spine was normal. She had full flexion of both hips with symmetrical internal rotation of about 60 degrees in the prone position. Hip impingement testing (flexing the hip to 90 degrees and then adducting and internally rotating it) produced significant pain; however, she had minimal to no pain with abduction and with external rotation. Results of a neurovascular examination of the right lower extremity were normal.
Radiographs were obtained. A standing anteroposterior (AP) view of the pelvis and bilateral false profile (25 degrees oblique) views of the hips revealed a dysplastic hip on the right side with mild coxa magna (slightly large femoral head compared with the left side) (Figure 1). The lateral center edge angle of the right hip was neutral, and the anterior center edge measured −5 degrees. Anterior and lateral coverage of the left hip, by contrast, was more than 25 degrees (which is the norm). There was minimal subluxation, and congruency between the femoral head and the acetabulum was maintained on radiography.
MRI of the affected hip revealed no distinct labral tear. There was no evidence of degenerative joint disease and no avascular change in the right femoral head.
The patient and her parents elected to postpone surgery until after she had completed her senior year of high school; she was instructed to return when she wanted to proceed. She returned 9 months later complaining of worsening pain.

DEVELOPMENTAL DYSPLASIA OF THE HIP: AN OVERVIEW
DDH refers to a spectrum of abnormalities involving the growing hip, including subluxation, dislocation, and alteration of the size, shape, or organization of the femoral head and/or acetabulum. It is estimated that DDH affects between 1 and 1.5 children for every 1000 births, with some studies showing as many as 9 of every 1000 children affected.1-3
The risk of DDH is much higher in girls, and firstborn children are affected twice as often as those later in the birth order. A child whose first-degree relative was affected by DDH has a slightly increased risk. Children with oligohydramnios, torticollis, clubfeet, or connective-tissue disorders are also at a higher risk.2 The left side is more often affected than the right side.1
There is also geographical and racial variation in the incidence of DDH. An increased incidence has been noted in North America and among Native Americans; in contrast, DDH is seldom seen among African American or Chinese children.1,2
The etiology of the disorder is multifactorial, with mechanical, hormonal, genetic, and various other mechanisms possibly playing roles. The risk of DDH is increased with intrauterine crowding or breech presentation and in neonates whose hips are held in an extended and adducted position while swaddled or wrapped. Maternal hormones can induce significant ligament laxity, which could explain the higher incidence of DDH in girls.
DIAGNOSIS OF DDH
Early diagnosis of DDH is important to prevent the long-term effects of untreated hip dysplasia, such as those seen in this teenager. Dysplasia that has gone unnoticed during childhood can result in degenerative arthritis by the teenage or young adult years.4 The ideal time to detect DDH is in the newborn period. When the disorder is diagnosed in infancy, treatment is effective more than 90% of the time.1-3
Developmental dysplasia of the hip (DDH) was diagnosed. It was explained to the patient and her family that a reconstructive procedure was indicated. The risks and benefits of the recommended procedure (a periacetabular osteotomy) were discussed, along with the typical preoperative and postoperative course.
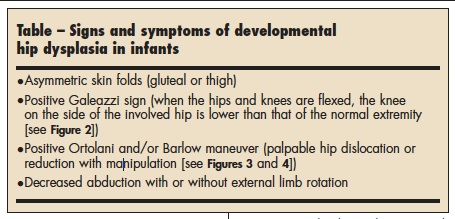
Often DDH can be picked up in a neonate with a routine history taking and physical examination. Signs and symptoms that suggest the diagnosis (Table) include asymmetric skin folds; the presence of a condition known to be associated with DDH, such as torticollis or clubfoot; and one knee lower than the other when the infant is in a supine position with hips and knees flexed (Galeazzi sign [Figure 2]).

Two maneuvers are also commonly used to detect DDH in infants. In the Ortolani maneuver, one hip is held in abduction while the other is gently manipulated to see whether the femoral head can be reduced into the acetabulum (Figure 3). In the Barlow maneuver, gentle downward pressure is applied to one hip to determine whether the femoral head can be dislocated from the acetabulum (Figure 4).1
When a clinical abnormality is detected in an infant up to 6 to 8 months of age—or when the history or other physical findings place an infant at high risk for DDH— ultrasonography of the hip(s) is warranted. Ultrasonography is preferred to radiographs in children younger than 6 months because the femoral head has not yet ossified, and cartilage and soft tissues are better delineated on an ultrasonogram. After age 6 months, plain AP and frog-leg pelvis radiographs are usually ordered. If imaging studies reveal any abnormality, refer the child to a pediatric orthopedist for evaluation.


INTERVENTIONS FOR DDH
Intervention in infants who have not yet begun to walk is by means of a hip abduction orthosis known as a Pavlik harness. As children reach walking age, casting with open or closed reduction of the hip is required. Any residual dysplasia is treated with surgical management using various reconstructive options.
Although infancy is the ideal time to intervene to correct DDH, surgical correction is often recommended at whatever age the condition is identified; residual dysplasia is a major cause of disability. The treatment of adolescents and young adults with hip disorders such as DDH has changed significantly over the past 10 years; these changes are the result of better understanding of prearthritic and early arthritic disease and of improved diagnostic skills and surgical procedures.5
Periacetabular osteotomy is quickly becoming one of the surgical interventions of choice in patients under the age of 40.5 Adults and adolescents in whom the triradiate cartilage is closed, whether or not they have had previous treatment or surgery, can benefit from a periacetabular osteotomy.6 The procedure produces a more normal configuration of the hip joint and improves load-bearing capacity; it thus arrests the degenerative process and may greatly improve hip joint longevity.6 In addition, periacetabular osteotomy leaves the posterior column intact, thereby maintaining stability in the pelvic ring— an advantage over other types of osteotomies, especially for women of childbearing age.7
OUTCOME OF THIS CASE
The patient underwent periacetabular osteotomy. She healed uneventfully; Figure 5, an AP radiograph of her pelvis 3 months after surgery, shows the healed osteotomy. At this point, she had very little pain. Her mobility continues to improve, and her risk for early degenerative arthritis is significantly reduced.



