Sleep is an important, yet frequently underestimated component of adolescent health. Adequate sleep is essential for achieving maximal cognitive abilities as well as for maintaining the energy needed to meet the demands of a busy adolescent’s schedule. Lack of quality sleep can result in attention problems, cognitive dulling, various somatic complaints (such as headaches and abdominal pain), and mood disturbances.
Here, I provide background information on adolescent sleep and then present 3 case reports that illustrate some of the more common teenage sleep problems. My hope is that the ensuing discussions will help practitioners reflect productively on issues of sleep and sleep hygiene that they may encounter in their adolescent patients.
WHY SLEEP?
 Sleep involves a complex series of physiological events that evolve throughout the lifespan. Various conflicting theories describe how the brain balances its need for sleep with its need for wakefulness. I like to use a model in which 2 parallel processes control the sleep-wake cycle. The first process involves biological homeostasis: the brain maintains an innate balance between sleep and wakefulness that is reset every morning when the person wakes up. As the day progresses, this homeostatic drive accumulates a “sleep need” that, by bedtime, compels the person to sleep and then resets the balance for the next morning. The second process involves a brain-based circadian rhythm that controls the production of melatonin(, cortisol, and other sleep-controlling hormones.
Sleep involves a complex series of physiological events that evolve throughout the lifespan. Various conflicting theories describe how the brain balances its need for sleep with its need for wakefulness. I like to use a model in which 2 parallel processes control the sleep-wake cycle. The first process involves biological homeostasis: the brain maintains an innate balance between sleep and wakefulness that is reset every morning when the person wakes up. As the day progresses, this homeostatic drive accumulates a “sleep need” that, by bedtime, compels the person to sleep and then resets the balance for the next morning. The second process involves a brain-based circadian rhythm that controls the production of melatonin(, cortisol, and other sleep-controlling hormones.
While pre-adolescents require 10 to 11 hours of sleep at night, adolescents entering puberty have a sleep requirement of 9 to 91⁄2 hours. Coincident with the decreased need for sleep is an approximately 2-hour physiological diurnal sleep phase delay (involving changes in both the homeostatic drive and melatonin secretion). Thus, a pre-teen who needed to go to bed by 9 or 10 at night might, as an adolescent, not experience the urge to sleep until 11 or 12.
One can see how external factors such as school, activities, sports, and after-school jobs can contribute to a chronic lack of sleep in adolescence. For example, many middle schools and high schools start their academic days at about 7:30 AM, which can result in students getting 6 to 7 hours of sleep, with subsequent sleep deprivation in many. Contrary to the beliefs of many parents and teens, the notion that one can “catch up on sleep” by sleeping until noon on the weekends is incorrect, and trying to do so may exacerbate sleep problems. From a sleep hygiene perspective, a relatively consistent sleep pattern is best.
Adolescent medicine providers frequently are asked to determine whether a teenager’s sleeping pattern is normal or suggestive of a sleep disorder. Some of the sleep problems commonly seen in adolescence include nightmares, nocturnal enuresis, and decreased sleep resulting from over-enrollment in activities. However, an adolescent’s physician must also be alert to the possibility of more severe disorders, such as sleep phase disorders, parasomnias (eg, sleepwalking), obstructive sleep apnea syndrome, and narcolepsy (Box).
The following 3 scenarios illustrate some of the more common adolescent sleep problems, and the accompanying discussions may provide insight into the sorts of issues you are likely to encounter.
Case 1: Fatigue Subsequent to Difficulty Falling Asleep at Night
Chris, 16 years of age, comes to the office in mid-September complaining of persistent daytime fatigue. His mother says that she has to drag him out of bed in the morning and remarks that since school began 4 weeks ago, he “just can’t get his act together” on school days. Teachers are concerned that Chris is falling asleep in class and is unable to function well academically this year. After school, he has soccer practice. He sometimes takes a 2-hour nap between 6 and 8 PM so that he has the energy needed to do his homework at night. Weekends tend to be less problematic because Chris can sleep until 12 or 1 in the afternoon.
The physical examination findings are unremarkable. Chris denies any new stresses or anxieties. When asked about his summer, he reports that he had a great summer and that he stayed up almost every night until 3 AM using the computer and talking to friends. The fatigue became a problem only when he had to start getting up for school at 6 AM. In response to the suggestion that he needs to get into bed by 10 PM with all extraneous stimuli, such as cell phone and computer, turned off, Chris counters that despite consistent attempts to go to bed earlier, he “just lies in bed until 3 AM, so why bother going to bed earlier?”
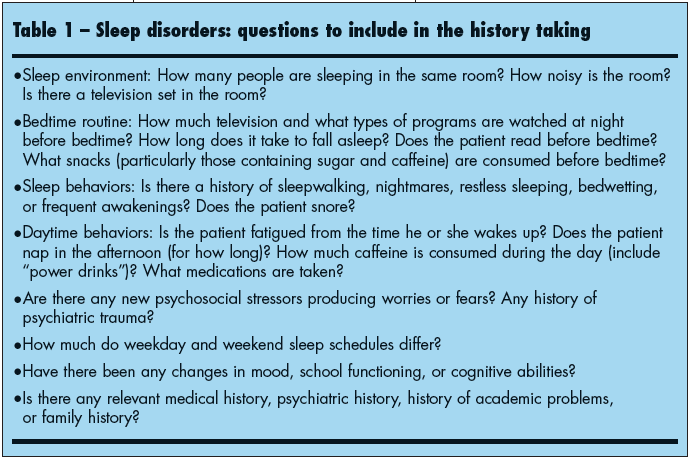 When evaluating a patient for a possible sleep disorder, it is important to elicit a comprehensive sleep history. Examples of questions to ask are shown in Table 1. If there is any uncertainty, you can ask the patient and family to complete a sleep diary, which includes daytime fatigue levels, time spent napping, time of “lights out,” approximate time of sleep onset, activity during the day and before sleep, and time of awakening.
When evaluating a patient for a possible sleep disorder, it is important to elicit a comprehensive sleep history. Examples of questions to ask are shown in Table 1. If there is any uncertainty, you can ask the patient and family to complete a sleep diary, which includes daytime fatigue levels, time spent napping, time of “lights out,” approximate time of sleep onset, activity during the day and before sleep, and time of awakening.
Chris likely suffers from delayed sleep phase syndrome (DSPS). DSPS frequently occurs after long periods in which the sleep-wake cycle is delayed by more than 2 hours, such as during summer vacations. Although sleep onset is delayed, the sleep quality tends to be normal (as evidenced by polysomnography). However, the teenager who cannot readjust to a normal sleep routine, as is required by a school schedule, will eventually demonstrate signs and symptoms of sleep deprivation. These may include headaches, daytime fatigue, irritability, emotional lability, and cognitive/ attentional deficits.
Which interventions will most effectively reset a diurnal schedule depend on the amount of time between the desired and actual sleep onset times. When sleep onset is less than 2 hours later than the desired bedtime (a bedtime that would provide the ideal 9 hours of sleep), then one can simply attempt to advance both the bedtime and the wake time by approximately 15 minutes every night until the bedtime and sleep onset time coincide. For example, if a patient cannot fall asleep until 1 AM but has been sleeping until 10 AM, you can recommend that the bedtime be advanced to 12:45 AM, then 12:30 AM, then 12:15 AM, and so forth, with concurrent wake times of 9:45, 9:30, and 9:15 AM, until the desired sleep schedule is reached. Ideally, I would recommend beginning this process at least 1 week before the start of a new school year or job. For the duration of this treatment, napping should be minimized to 30 minutes a day at most.
However, patients such as Chris, whose sleep onset is 3 hours (or more) later than the desired sleep time, probably need to undergo home-based chronotherapy. This treatment is time- and labor-intensive for the family, but it has been shown to be effective in treating DSPS. It involves progressively delaying the sleep phase by 3 hours per night until the desired bedtime is reached. Thus, I would instruct Chris and his family to delay bedtime (and wake time) by approximately 3 hours every day. He would need to keep himself up until 6 AM, 9 AM, 12 PM, and so forth, and would have to wake up at 3 PM, 6 PM, 9 PM, respectively. During this therapy, napping is forbidden and stimulant drinks should be avoided. Once he reaches the desired schedule, Chris must maintain the schedule (give or take 30 minutes) on weekends to avoid a relapse.
Phototherapy is another effective treatment for DSPS. However, it tends to be a more complicated intervention and is beyond the scope of this article. If chronotherapy fails and phototherapy is required, I generally refer the patient to a sleep disorder specialist.
Many clinicians wonder whether melatonin might be a potential treatment in situations such as this. The adult literature demonstrates that melatonin shifts circadian phases, and if given 15 to 20 minutes before the desired bedtime, it will enhance phase advances. However, the efficacy and safety of melatonin in adolescents and children are untested. At present, exogenous melatonin is not FDA-approved for children or adolescents with DSPS.
Outcome of this case: Chris underwent chronotherapy with the support of his parents. After 4 or 5 days, he had adjusted to a schedule in which he went to sleep at 10:30 PM and awoke at 6 AM. From the end of September through December, his school performance was improved. Unfortunately, during the 2-week winter vacation he began once again habitually staying up late and sleeping until 1 PM. Thus, 3 days before he had to go back to school, Chris and his parents needed to repeat chronotherapy to get him back on an appropriate schedule.
Case 2: Headaches and Unrefreshing Sleep in a Snorer
Fourteen-year-old Trevor, who has been extremely healthy, comes in for an annual athletic physical. Although he insists that he has no physical complaints, his mother interjects, “Trevor, I thought you wanted to tell the doctor about your headaches! Doctor, he complains at least 4 or 5 times a week that his head hurts, and he is always tired. Last week, he missed the bus twice because it was so hard to get him out of bed. Oh, and while we are on this subject, is there any pill you can give him to make him stop snoring? My room is across the hall, and I can’t sleep unless I keep my head under a pillow!”
Speaking privately with his physician, Trevor sheepishly admits that he has been feeling tired a lot lately and that he often takes a 2- hour nap in the afternoon; however, the naps don’t make him feel less tired. He goes to sleep exhausted at 10 PM and sleeps until 7 AM, but he doesn’t feel refreshed in the morning. If he sleeps until 10 or 11 AM on the weekends, he feels a little bit better but still needs an afternoon nap. Trevor admits he has headaches, which usually occur in the afternoon. He denies visual changes, photophobia, and vomiting with the headaches. The headaches are usually bilateral and “squeezing” in quality.
Trevor denies any other physical complaints, symptoms of depression, and drug use. His grades have not been as good over the past year because he has a hard time concentrating in school, and his teachers have recommended that he be evaluated for attention-deficit/hyperactivity disorder (ADHD).
The results of a comprehensive physical examination, including neurological examination, are normal. Trevor’s fundal discs are sharp. His height and weight are both at the 60th percentile. The only notable finding is some moderately enlarged bilateral tonsillar tissue, which has been noted numerous times in the chart. Trevor denies any sore throat.
In the past, many clinicians might have counseled Trevor and his mother that teenagers are always tired and that feeling tired is part of being an adolescent. However, this scenario has certain features that are more troubling. First, Trevor appears consistently fatigued even when he gets 9 or more hours of sleep at night. Even a substantial afternoon nap does not seem to help him feel better. Another notable feature is that his teachers have noticed an objective, gradual decline in his academic abilities, to the degree that they want him evaluated for ADHD.
 Might Trevor have a syndrome of sleep-disordered breathing, such as obstructive sleep apnea (OSA)? Patients with this condition frequently have difficulties with air inspiration during sleep, because the musculature supporting a patent airway (at the level of the nose, palate, or hypopharynx) collapses when they fall asleep. The resulting obstruction leads to an increase in inspiratory effort and hypoxemia. This frequently results in increased wakefulness that disrupts healthy sleep architecture. While patients may not be aware of these symptoms, they will experience symptoms of sleep deprivation. The signs and symptoms of OSA are outlined in Table 2.
Might Trevor have a syndrome of sleep-disordered breathing, such as obstructive sleep apnea (OSA)? Patients with this condition frequently have difficulties with air inspiration during sleep, because the musculature supporting a patent airway (at the level of the nose, palate, or hypopharynx) collapses when they fall asleep. The resulting obstruction leads to an increase in inspiratory effort and hypoxemia. This frequently results in increased wakefulness that disrupts healthy sleep architecture. While patients may not be aware of these symptoms, they will experience symptoms of sleep deprivation. The signs and symptoms of OSA are outlined in Table 2.
In this case, the historical feature that piques my interest the most is the patient’s snoring. His loud snoring bothers Trevor’s mother so much that she wants medication to fix it! It would be important to ask family members about the quality of the snoring: How loud is it? Is it rhythmic or disjointed sounding? Does it ever sound like Trevor stops breathing for a period, followed by a gasping breathing pattern?
While many used to believe that OSA only occurred in overweight and obese persons, we now know that this is not the case. The American Academy of Pediatrics recommends that pediatricians screen all children and adolescents for a significant history of snoring and that they consider polysomnography (sleep study) in those who snore—regardless of body habitus—to evaluate for sleep apnea. In many persons, such as Trevor, upper airway obstruction can be caused solely by anatomical abnormalities, such as large tonsils or adenoids.
Outcome of this case: Trevor underwent polysomnography, which demonstrated multiple obstructive apneic episodes throughout the night, occasionally with oxygen desaturations into the mid-80s (%), clinching the diagnosis of OSA. He was referred to an otolaryngologist who eventually removed his tonsils. His snoring almost immediately disappeared, and a follow-up sleep study demonstrated complete resolution of the apneic events. Moreover, Trevor’s energy and grades dramatically improved.
It should be noted that surgical corrections for OSA are not universally effective. The gold-standard treatment is continuous positive airway pressure (CPAP), especially for the more “classic” obese patient with OSA. However, many children and adolescents do not tolerate CPAP administration and may elect a surgical option if one is appropriate.
Case 3: Low Energy, Loss of Appetite, and Difficulty in Sleeping
Fifteen-year-old Melanie just finished her freshman year in high school. She comes to the office to have a tuberculin skin test and physical clearance for a job at a summer camp. You notice that she looks tired, and she admits that she has been having trouble sleeping. Melanie relates that she tries to go to sleep as early as 9 PM, but she usually lies in bed, thinking about her life, for at least 2 to 3 hours. She sets her alarm for 7 AM, but often spontaneously wakes up as early as 5 AM (or even earlier) and cannot fall back asleep. She denies any new stresses that might be keeping her awake, but she does relate that almost 1 year ago, her best friend was killed in a car accident (Melanie was in the car) and that she has been thinking about the incident a lot.
Melanie admits that she feels guilty that she survived the accident while her friend did not. She states that over the past few months, her energy levels have dwindled and that she “just does not have the energy to go out with her friends.” She spends a lot of time by herself in her room, writing poetry. Her mother has been concerned that she is losing weight, and she admits that she has a poor appetite. She wishes that she could get back to feeling the way she used to.
She denies any drug, alcohol(, or caffeinated beverage use. When told, “It must be really difficult to have all this going on inside. You’re dealing with so much at once, no wonder you can’t sleep,” Melanie starts to cry.
Research regarding adolescent emotional health has demonstrated bidirectional relationships between emotional state and the quality of sleep. Children and adolescents with anxiety disorders, depression, and bipolar disorders frequently have difficulty establishing and maintaining sleep on a regular basis. Conversely, teenagers who are sleepdeprived frequently report mood disturbances. Although attempts to determine the true cause in a given patient may seem futile—turning up little more than a classic “chickenand- egg” situation—it is also possible (and even likely) that poor-quality sleep and poor emotional health concurrently worsen each other.
When evaluating patients with sleep problems, always screen for psychiatric problems. Anxiety disorders frequently cause insomnia, with increased time to fall asleep and difficulty reaching deep (stage 3/4) sleep. Theoretically, a sense of security is needed to achieve a deep sleep. The absence of that degree of security precludes the ability to achieve deep and restful sleep, thus giving the anxious adolescent chronic complaints of fatigue and insomnia.
Melanie demonstrates features consistent with major depressive disorder (MDD): more than 2 weeks of depressed mood, anhedonia, sleep disturbance, loss of appetite, feelings of guilt and worthlessness, and lack of energy. Other signs and symptoms that would be consistent with MDD include decreased concentration, psychomotor retardation (or agitation), and suicidal ideation.
A comprehensive discussion about treatments for depression is beyond the scope of this article. Suffice it to say, if you suspect depression or any mood disorder as the cause of sleep disturbance, the patient should be evaluated and treated by a psychiatrist or other specialist experienced with these issues. Before referral, inquire about any suicidal ideation and, if present, request an immediate psychiatric evaluation.
In general, treatment may consist of psychotherapy, antidepressant medication, or a combination of these 2 modalities. Some of the adult sleep literature suggests that depression-related insomnia should be treated with hypnotic agents (such as zolpidem() as an adjunct to the treatment of depression. However, I would caution against the use of these medications until their safety and efficacy in adolescents have been established.
Outcome of this case: Melanie denied any suicidal intentions, and she promised to immediately tell her mother if she began to have suicidal thoughts. She was referred to an adolescent psychiatrist who, after a comprehensive evaluation, diagnosed MDD and initiated therapy with a selective serotonin reuptake inhibitor. She also began counseling with a psychologist who specialized in depression and grief. After 3 to 4 weeks, her mood and her sleep patterns gradually began to improve. About 2 months later, Melanie’s mother reported that her daughter was “getting back to her old self.”


