Ileoileal Intussusception With Severe Bruxism and Mandibular Osteomyelitis
A 23-month-old Korean boy with no significant medical history presented to the pediatric emergency department (ED) after 5 of his bottom teeth fell out. His father reported that on the previous night, the boy began to have a new onset of severe bruxism along with several episodes of nonbloody, nonbilious emesis. There was no associated fever or diarrhea.
The boy had been born in the United States but had lived in South Korea for 1 year until 4 months prior to presentation, when the family had moved back to the United States.

On initial examination, the child was afebrile and normotensive but with notable mild tachycardia. He was well-developed and well-nourished. He had 5 missing bottom teeth, with gray, friable gums (A). His abdomen was soft and mildly tender to palpation diffusely but not distended. No masses or organomegaly were appreciated. Normal bowel sounds were auscultated.
A dentistry consultant evaluated the patient in the ED and reported that the boy had necrotic mandibular tissue but healthy teeth. The patient subsequently was admitted for administration of intravenous antibiotics and further workup.
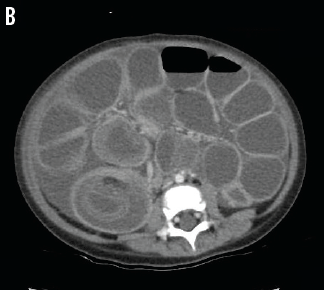
During the first 24 hours of his hospital course, the patient had an unexplainable drop in hemoglobin concentration that was followed by abdominal distention and then bloody diarrhea. A stat abdominal computed tomography scan with contrast was performed, which demonstrated the presence of an ileoileal intussusception (B).
The patient was immediately taken to the operating room, where the surgical team removed 20 cm of small bowel and created an ileostomy. During the operation, a pathologic lead point of a hamartomatous polyp was identified and excised. The patient did well postoperatively and was continued on a prolonged course of systemic intravenous antibiotic therapy for mandibular osteomyelitis.
 Intussusception occurs when a segment of bowel telescopes into a more distal segment. This leads to obstruction of venous return and subsequent edema and engorgement. Following this, arterial blood flow eventually becomes obstructed, causing bowel ischemia. This leads to bleeding from the mucosa and mucosal shedding, which form the classic “currant jelly” stool. Complications can include gut ischemia, intestinal gangrene, shock, and death.1
Intussusception occurs when a segment of bowel telescopes into a more distal segment. This leads to obstruction of venous return and subsequent edema and engorgement. Following this, arterial blood flow eventually becomes obstructed, causing bowel ischemia. This leads to bleeding from the mucosa and mucosal shedding, which form the classic “currant jelly” stool. Complications can include gut ischemia, intestinal gangrene, shock, and death.1
Intussusception is the most common cause of bowel obstruction in children between 4 and 10 months of age.2 One literature review of pediatric intussusception demonstrated a worldwide mean incidence of 74 per 100,000 children younger than 1 year of age.3
The typical presentation of intussusception includes a sudden onset of severe, intermittent abdominal pain with pain-free time intervals. Pediatric patients may present with flexion of the lower extremities and crying. With worsening intestinal ischemia, the patient may become lethargic and progress to shock. The classic triad of abdominal pain, palpable sausage-shaped mass, and currant jelly stool present in less than 15% of patients with intussussception.1
Our patient’s presenting symptoms were the acute onset of bruxism and episodes of emesis. It is unclear how and whether the patient’s mandibular osteomyelitis and intussusception are related. To date, there are no known case reports of intussusception associated with osteomyelitis.
References
1. Kennedy M, Liacouras CA. Intussusception. In: Kliegman RM, Stanton BF, St. Geme JW III, Schor NF, Behrman RE, eds. Nelson Textbook of Pediatrics. 19th ed. Philadelphia, PA: Elsevier Saunders; 2011:1287-1288.
2. World Health Organization. Acute intussusception in infants and children: incidence, clinical presentation and management: a global perspective.
http://whqlibdoc.who.int/hq/2002/WHO_V&B_02.19.pdf. Published October 2002. Accessed January 19, 2015.
3. Jiang J, Jiang B, Parashar U, Nguyen T, Bines J, Patel MM. Childhood intussusception: a literature review. PLoS One. 2013;8(7):e68482.


