ABSTRACT: Head shape abnormalities in infants may be the result of pressure on the malleable bones in the newborn skull during a vaginal delivery (molding), of constant gravitational forces on the occiput when an infant is kept in the same supine position for prolonged periods (positional deformational plagiocephaly), or of premature fusing of one or more of the cranial sutures (craniosynostosis). Craniosynostosis is by far the rarest of these 3 etiologies. Head shape abnormalities caused by molding usually disappear within the first few weeks of life. Those that persist beyond this time or become apparent later require a thorough workup that includes a medical and family history, various skull measurements, checking for torticollis, and careful palpation of the head and neck. Skull radiographs can rule out craniosynostosis in infants with pronounced shape abnormalities. Deformational plagiocephaly is usually treated with repositioning therapy or, in more severe or recalcitrant cases, helmet therapy. To prevent this disorder, advise parents to provide their child with at least 5 minutes of "tummy time" daily. The need for surgery to correct craniosynostosis depends on the severity and extent of associated deformities.
________________________________________________________________________________________________________________________________________________
"Does my baby's flat head mean he has to wear a helmet?" That question, recently posed by a concerned parent, is typical of the inquiries pediatricians hear regularly about head shape abnormalities. How would you respond to this parent's concern?
Here we offer a practical, objective approach to determining which patients with odd head shapes require further evaluation and treatment.
CAUSES OF HEAD SHAPE ABNORMALITIES IN INFANTS
Odd head shapes develop because the bones of the newborn skull are moveable and malleable. The bones are able to move because they are adjoined by fibrous sutures (junctures between 2 bones) and fontanelles (junctures between more than 2 bones) that remain unossified throughout the first years of life to facilitate vaginal delivery and allow expansion of the growing brain. The anterior fontanelle, easily palpated at the top of the head, typically closes by 18 to 24 months of age. The posterior fontanelle is more difficult to appreciate on physical examination and often closes in the first few months of life.
The major forces that misshape the head include:
• External pressure, either applied to the skull during the birthing process or resulting from uterine constraint in cases of multiple births (molding).
• Gravitational forces applied to the skull during early infancy (deformational or positional plagiocephaly).
• Early fusion of one or more of the sutures (craniosynostosis [Figure 1]).
Molding. In utero, molding can result from uterine crowding, such as occurs when multiple fetuses share the same womb. During parturition, the strong forces applied to the skull as it is squeezed through the birth canal cause the bones that make it up to override one another; this process can "mold" the head into various shapes. Difficult deliveries that require the use of forceps or vacuum extraction can result in severe molding. In addition, the calcification of a healing cephalohematoma can produce a distinct lump on the skull, usually on one of the parietal convexities. When discovered by a concerned parent (usually when the child is 1 to 2 months old), such a lump often prompts a visit to the pediatrician. Reassure parents that a cephalohematoma poses no long-term risk.
Because molding secondary to the birthing process typically resolves in hours to weeks, persistent or progressive shape deformities beyond that time should raise suspicion for deformational plagiocephaly or craniosynostosis.
 |
| Figure 1 – A normal newborn’s skull consists of several plates of bone that are joined by fibrous sutures that facilitate vaginal delivery and expansion of the growing brain. In craniosynostosis, one or more of the sutures close prematurely, causing problems with normal brain and skull growth and resulting in an abnormal, asymmetric appearance. There are numerous types of craniosynostosis, each of which involves a different suture or combination of sutures and results in a distinctive head shape. Three of the more common types are shown here. (Reprinted with permission from: University of Utah Health Sciences Center. Craniofacial Anomalies. Available at: http://uuhsc. utah.edu/healthinfo/pediatric/craniofacial/cranio.htm.) |
Deformational plagiocephaly. Posterior-type deformational plagiocephaly is caused by constant gravitational forces applied to the occiput when the infant remains for prolonged periods in the same supine position--the sleep position promoted by the American Academy of Pediatrics (AAP) Back to Sleep campaign (Figure 2).1 Various degrees of brachycephaly (ie, a shortened, broad head) occur in most children who sleep solely on their backs.2
Any condition that is associated with abnormal bone formation or muscle tone (especially torticollis) can also cause deformational plagiocephaly. Dolichocephaly (ie, a long, narrow head with bitemporal narrowing) can develop in preterm infants who have large heads and weak neck muscles.3
 |
| Figure 2 – The incidence of occipital plagiocephaly has risen dramatically since the AAP suggested the supine sleep position. (Reprinted with permission from: Losee JE, Feldman E, Ketkar M, et al. Nonsynostotic occipital plagiocephaly: radiographic diagnosis of the "sticky suture." Plast Reconstr Surg. 2005;116: 1860-1869.) |
Craniosynostosis. Exactly why sutures fuse early is not known, but genetic and environmental factors--such as single gene mutations, teratogen exposure, and fetal constraint--probably play a role.4 Craniosynostosis may also be an associated feature of several genetic syndromes, including Apert, Crouzon, Dubowitz, and Treacher Collins-Franceschetti syndromes.
Crouzon syndrome is associated with various facial and skull deformities, exophthalmos, and hydrocephalus. Apert syndrome is also associated with significant craniofacial deformities, hydrocephalus, and exophthalmos, along with mental retardation and syndactyly. Dubowitz syndrome5 is associated with marked microcephaly and facial anomalies (as well as other features); Treacher Collins-Franceschetti syndrome6 is associated with severe craniofacial abnormalities and hearing loss.
When craniosynostosis occurs, the growth of the skull is impeded in a plane that is perpendicular to the fused suture, but the skull continues to grow in the parallel plane. Brain growth occurs in the direction of the open sutures. Different head shapes result (see Figure 1) depending on which suture or combination of sutures has fused:
• Trigonocephaly (a triangular-shaped head) arises from metopic craniosynostosis.
• Scaphocephaly arises from sagittal craniosynostosis.
• Turricephaly (a tower-shaped head) arises from coronal plus sagittal craniosynostosis.
• Brachycephaly arises from bilateral coronal craniosynostosis.
• Posterior plagiocephaly (trapezoidal-shaped head) arises from lambdoid craniosynostosis; this is a very rare form of craniosynostosis.
EPIDEMIOLOGY
Hutchison and colleagues7 found that head shape in otherwise normal children varies to a great extent in the first 2 years of life and that misshapen heads eventually improve as infants age. Many, if not most, newborns display some degree of molding, especially if born via a vaginal delivery.
Among children beyond the immediate newborn period, a 2004 report revealed that approximately 1 in 68 infants displays significant cranial asymmetry from positional or deformational plagiocephaly.8 This is significantly higher than the 1 in 300 rate typical in decades past; the increase correlates with the initiation of the AAP Back to Sleep campaign in 1992.8,9
Craniosynostosis occurs much less frequently--in an estimated 1 in 2000 live births.10 Lambdoid craniosynostosis is even more uncommon; the estimated incidence is 1 in 300,000 births,9 although it is suspected far more frequently than this because it is easily confused at first observation with deformational plagiocephaly. Huang and coworkers11 reported a 3% incidence of unilateral lambdoid craniosynostosis in their series of patients who were referred for plagiocephaly and craniosynostosis.
(Continued on next page)
EVALUATION
History and review of systems. The evaluation of the child with an odd head shape begins with a thorough history taking (Table 1). It is important to ascertain the age at onset and the circumstances of birth and gestation (eg, singleton vs multiples, premature vs full-term delivery, vaginal vs cesarean delivery). An odd-shaped head in a newborn is most likely the result of molding; more severe shape abnormalities (as well as bruising and scalp swelling) are especially likely to be associated with a forceps or vacuum-extracted vaginal delivery. Changes secondary to molding improve in the first hours to weeks of life.
The persistence or worsening of an abnormal head shape beyond the newborn period is worrisome. When this occurs, you must determine whether the cause is craniosynostosis (isolated or syndrome-associated) or deformational plagiocephaly.
In cases of persistent or worsening head shape deformity, it is important to inquire about family history of odd head shapes, craniosynostosis, dysmorphic features, and suspected or known genetic syndromes. Record developmental milestones and conduct a thorough review of systems, with a focus on neurologic or ophthalmologic abnormalities and signs of torticollis or occipital hair loss. Be sure to ascertain the amount of time that the baby spends in the supine versus the prone position. Strongly suspect deformational plagiocephaly if the baby spends the majority of the day and night supine.7,12 Less than 5 minutes per day of "tummy time" in the first 6 weeks of life puts a child at particular risk for a flattened head.12
Physical examination. A thorough physical examination begins with observation of the child for any dysmorphic features, facial and head asymmetry, or head tilting. Note the shape of the head from above and at various angles, examine the position of the ears and cheekbones, and assess active and passive head rotation. The presence of a head tilt or neck mass and the inability to move the head in one direction may indicate torticollis. Although lambdoid craniosynostosis is easily confused with deformational plagiocephaly, there are distinctive clinical differences between the 2 entities that can often enable you to distinguish between them on the basis of the physical examination (Table 2).
Measure the head circumference and plot it, along with all growth parameters, on appropriate growth curves. Obtaining parental head size may also aid in the evaluation.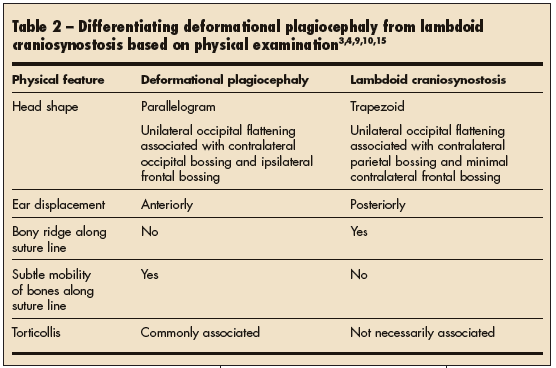
Two other measurements that may help with objective determination of whether the head shape is problematic include the cranial index (CI) and the diagonal difference (DD).2,13 The CI is the width of the head divided by its length, with the resulting fraction expressed as a percentage. Normal values range from 76% to 81%.2 A value of greater than 81% constitutes brachycephaly. The DD is the difference between the measured distance from the left occiput to the right forehead and that from the right occiput to the left forehead. For healthy infants aged 4 to 12 months, the normal DD is about 0.2 to 0.4 cm. A DD that approaches 1 cm or more, especially in an infant older than 6 months, constitutes severe plagiocephaly that warrants further investigation and may require aggressive intervention.13
Palpation of the skull is important to determine whether the fontanelles and sutures have fused. Bony ridges along suture lines or inability to palpate the "soft spot" at the top of the head suggests craniosynostosis. In the rare event that the anterior fontanelle is found to be closed in the first few months of life, you will need to decide how aggressive a workup is warranted. Piatt14 suggests that early closure of the anterior fontanelle and the presence of ridges along the suture lines are of no clinical significance if the overall head shape is normal and the head is growing normally.
Laboratory and imaging studies. The need for further laboratory or radiographic studies must be decided on a case-by-case basis. No laboratory studies are routinely obtained in the evaluation of the child with a misshapen head unless underlying bony or metabolic disorders are suspected (ie, rickets, vitamin D deficiency, renal disease, hyperthyroidism, or hypophosphatemia). When you suspect one of these latter disorders, consider obtaining serum levels of thyroid-stimulating hormone, alkaline phosphatase, vitamin D substrates, calcium, magnesium, and phosphorous--as well as a urinalysis.
Radiologic studies are not always needed. In a child with obvious mild deformational plagiocephaly, no further studies are necessary except when torticollis is present; in the latter case, consider obtaining a cervical spine series to rule out a cervical spine defect. However, monthly follow-up of affected children for the first several months of life is important to ensure normal head growth and improvement in head shape, normal development, and normal neurologic and ophthalmologic function. Order a skull radiograph if a child with suspected deformational plagiocephaly has not improved after 4 to 8 weeks of conservative therapy.15
If moderate or severe shape abnormalities are present, or if the definitive diagnosis is in doubt, then skull radiographs are a relatively inexpensive and safe test that can rule out craniosynostosis. The radiologic finding of bridging of bone or sclerosis over the suture or an indistinct suture line suggests craniosynostosis.16 If you are inexperienced in the interpretation of skull films, consult a pediatric radiologist. (Piatt14 advises that if you cannot make the diagnosis in the office, then direct referral to a pediatric neurosurgeon or a craniofacial clinic for consultation may be more reliable and cost-effective than ordering further imaging studies.) If the diagnosis is still in doubt or neurologic abnormalities are present, order a CT scan to determine definitively whether sutures have fused and whether brain anatomy is normal.
(Continued on next page)
MANAGEMENT
Craniosynostosis. In children with documented or suspected craniosynostosis, prompt referral to a pediatric craniofacial or neurosurgical expert is indicated (Table 3). The need for surgical intervention is decided on a case-by-case basis and depends on the severity and extent of associated deformities. Blindness, developmental delay, mental retardation, and elevated intracranial pressure are the most serious possible sequelae of craniosynostosis. Syndromic craniosynostosis may be especially worrisome on account of other associated features of the particular syndrome. For example, a child with Crouzon syndrome will require multidisciplinary care involving various surgical subspecialists (ie, a plastic surgeon and/ or neurosurgeon, ophthalmologist, otolaryngologist), a speech therapist, and an orthodontist.
Nonsyndromic craniosynostosis is also associated with cognitive, speech, and behavioral abnormalities.17 However, unlike in children with an associated syndrome or multisuture synostosis, it is uncommon for children who have nonsyndromic craniosynostosis to experience increased intracranial pressure.4 Ophthalmologic abnormalities associated with craniosynostosis include astigmatism and strabismus.18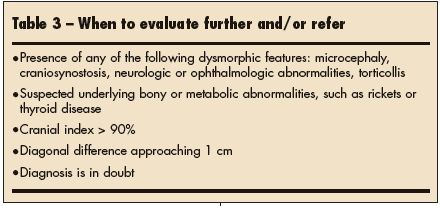
Deformational plagiocephaly. Although less worrisome than craniosynostosis, deformational plagiocephaly may require treatment as well; some affected children are at risk for future complications. Long-term sequelae may include a persistent abnormal head shape, facial asymmetry, and astigmatism.13,18 Gupta and colleagues18 found that 15% of their patients with deformational plagiocephaly had bilateral astigmatism and 9% had unilateral astigmatism. However, whether or not children with deformational plagiocephaly are at greater risk for the development of astigmatism than the general population has yet to be determined.18
Most mild cases of odd head shape will improve and become imperceptible as the child grows to maturity; severe cases may persist into adulthood to varying degrees. The true adverse developmental and emotional effects of abnormal head shape and facial asymmetry are unknown.15
Recommend strict adherence to the repositioning techniques outlined in Table 4 at the first sign of any occipital flattening.2 In more severe or persistent cases, helmet therapy or, rarely, surgery may be required. Craniofacial surgeons and pediatric neurosurgeons have the crucial role of determining the optimal management for a particular patient. Molding helmet therapy may be necessary if repositioning and physical therapy do not improve the situation. Keep in mind that helmet therapy is most effective in infants between 4 and 12 months9 of age. Such therapy may be a more effective initial treatment than repositioning,13 but there is no consensus yet.19
Suggested reasons for helmet therapy include:
• Progression or lack of improvement after 2 to 3 months of repositioning and physical therapy or if the child is older than 6 months.9
• A CI that exceeds 90% at age 5 months1 or a DD that is greater than 1 cm at age 6 months.13
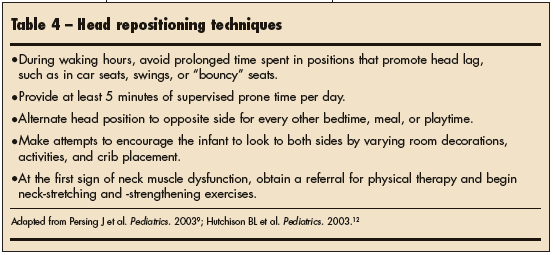
PREVENTION
With regard to deformational plagiocephaly, it is important to stay ahead of the game by counseling new parents about the importance of at least 5 minutes of supervised prone time per day for their baby. The Back to Sleep campaign has been successful and its virtues should continue to be touted--right along with the virtues of these simple plagiocephaly prevention measures.
REFERENCES:
1. Losee JE, Feldman E, Ketkar M, et al. Nonsynostotic occipital plagiocephaly: radiographic diagnosis of the "sticky suture." Plast Reconstr Surg. 2005;116: 1860-1869.
2. Graham JM Jr, Kreutzman J, Earl D, et al. Deformational brachycephaly in supine-sleeping infants. J Pediatr. 2005;146:253-257.
3. Huang MH, Mouradian WE, Cohen SR, Gruss JS. The differential diagnosis of abnormal head shapes: separating craniosynostosis from positional deformities and normal variants. Cleft Palate Craniofac J. 1998;35:204-211.
4. Ridgway EB, Weiner HL. Skull deformities. Pediatr Clin N Am. 2004;51:359-387.
5. Johns Hopkins University. Dubowitz syndrome. In: Online Mendelian Inheritance in Man. Available at:http://www.ncbi.nlm.nih.gov/entrez/ dispomim.cgi?id=223370. Accessed October 6, 2006.
6. Johns Hopkins University. Treacher Collins- Franceschetti syndrome. In: Online Mendelian Inheritance in Man. Available at:http://www.ncbi. nlm.nih.gov/entrez/dispomim.cgi?id=154500. Accessed October 6, 2006.
7. Hutchison BL, Hutchison LA, Thompson JM, Mitchell EA. Plagiocephaly and brachycephaly in the first two years of life: a prospective cohort study. Pediatrics. 2004;114:970-980.
8. Littlefield TR, Saba NM, Kelly KM. On the current incidence of deformational plagiocephaly: an estimation based on prospective registration at a single center. Semin Pediatr Neurol. 2004;11: 301-304.
9. Persing J, James H, Swanson J, Kattwinkel J. Prevention and management of positional skull deformities in infants. American Academy of Pediatrics Committee on Practice and Ambulatory Medicine, Section on Plastic Surgery and Section on Neurological Surgery. Pediatrics. 2003;112:199-202.
10. Kabbani H, Raghuveer TS. Craniosynostosis. Am Fam Physician. 2004;69:2863-2870.
11. Huang MH, Gruss JS, Clarren SK, et al. The differential diagnosis of posterior plagiocephaly: true lambdoid synostosis versus positional molding. Plast Reconstr Surg. 1996;98:765-774.
12. Hutchison BL, Thompson JM, Mitchell EA. Determinants of nonsynostotic plagiocephaly: a case-control study. Pediatrics.2003;112:e316-e322.
13. Graham JM Jr, Gomez M, Halberg A, et al. Management of deformational plagiocephaly: repositioning versus orthotic therapy. J Pediatr. 2005;146: 258-262.
14. Piatt JH Jr. Recognizing neurosurgical conditions in the pediatrician's office. Pediatr Clin N Am. 2004;51:237-270.
15. Biggs WS. Diagnosis and management of positional head deformity. Am Fam Physician. 2003;67: 1953-1956.
16. Kiesler J, Ricer R. The abnormal fontanel. Am Fam Physician. 2003;67:2547-2552.
17. Becker DB, Petersen JD, Kane AA, et al. Speech, cognitive, and behavioral outcomes in nonsyndromic craniosynostosis. Plast Reconstr Surg. 2005;116:400-407.
18. Gupta PC, Foster J, Crowe S, et al. Ophthalmologic findings in patients with nonsyndromic plagiocephaly. J Craniofac Surg.2003;14:529-532.
19. Bialocerkowski AE, Vladusic SL, Howell SM. Conservative interventions for positional plagiocephaly: a systematic review. Dev Med Child Neurol. 2005;47:563-570.
20. University of Utah Health Sciences Center. Craniofacial Anomalies. Available at: http://uuhsc. utah.edu/healthinfo/pediatric/craniofacial/cranio.htm Accessed October 16, 2006.
EVIDENCE-BASED MEDICINE:
• Ridgway EB, Weiner HL. Skull deformities. Pediatr Clin N Am. 2004;51:359-387.
• Persing J, James H, Swanson J, Kattwinkel J. Prevention and management of positional skull deformities in infants. American Academy of Pediatrics Committee on Practice and Ambulatory Medicine, Section on Plastic Surgery and Section on Neurological surgery. Pediatrics. 2003;112:199-202.


