Prescribing Exercise for Older Men
Introduction
The benefits of exercise and physical activity on health are well known and seldom debated. The value of physical training has been recognized for more than 2400 years. The first nonreligious schools of higher learning, called “Gymnasiums,” were created in Ancient Athens. The curriculum included the study of language, philosophy, mathematics, and physical fitness training; their principle was “healthy minds in healthy bodies,” as described in Plato’s writings. In Ancient Rome, Galen attributed some of the illnesses common in the nobility to their sedentary lifestyles. We now know that regular exercise training has positive effects on insulin sensitivity, body composition, blood pressure, cardiovascular and pulmonary function, lipid profile, bone mineral density, muscle strength and power, cognitive function, and chronic inflammation. All of these parameters show signs of deterioration with aging. Exercise is therefore a powerful intervention strategy to prevent or minimize the physiological changes associated with aging and to improve general health. In conjunction with diet, exercise is often the recommended first line of defense in the treatment and prevention for chronic diseases, such as cardiovascular disease, diabetes, and cognitive impairment. In fact, some epidemiological evidence shows that lack of physical activity is a greater risk factor for coronary heart disease than obesity, high cholesterol, family history, or hypertension.1 In addition, it has been shown that middle-aged adults who adopt a healthy lifestyle (regular exercise, 5 or more fruits and vegetables daily, maintaining healthy weight and no current smoking) receive a quick return on their investment in terms of significantly reduced all-cause mortality and 35% lower risk for cardiovascular disease after 4 years.2
What is less established is determining what kind of exercise programs are optimal for older adults. In 2007, the American College of Sports Medicine (ACSM) and the American Heart Association (AHA) published recommendations for physical activity in older adults.3 Older adults were defined as men and women 65 years of age or older and adults age 50-64 years with clinically significant chronic conditions and/or functional limitations. These guidelines emphasized reducing sedentary behavior in older adults, increasing moderate activity including muscle-strengthening activity, and defining moderate- versus high-intensity. An overview of these recommendations is shown in Table I.

In this article we will attempt to provide clinicians with information in the areas of exercise and lifestyle modifications that are specifically designed to help prevent sarcopenia and increase physical function in older men. We will focus mainly on the importance of muscle power. We will also review the most common exercise-related injuries in older men and suggest measures that can minimize the risk for injury. Lastly, the role of growth hormone and other supplements as an adjunct therapy will be discussed. These guidelines are intended to assist clinicians in making specific recommendations to their patients as part of a comprehensive evaluation and treatment plan.
Muscular Function and Body Composition in Aging Men
Aging is associated with a gradual loss of skeletal muscle mass, usually called sarcopenia, which starts as early as age 25-30 years and continues at a more rapid rate after age 50. By the age of 80 years, approximately 50% of the muscle mass is lost. For the lower-extremity muscles, the loss of muscle strength is even greater than the loss of muscle mass, indicating reduced muscle quality. The greatest loss is observed for muscular power.4 Muscle power is a product of the force and velocity of muscle shortening and is, therefore, more relevant to the completion of many daily activities than muscle strength. Leg power has been shown to be the best predictor of functional status5 and physical performance.6,7
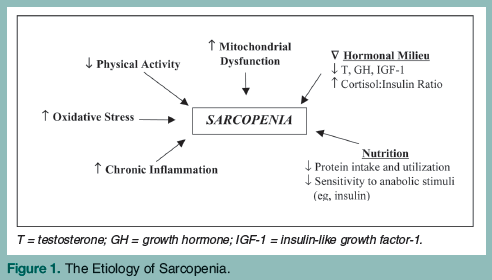
The etiology of sarcopenia is multifactorial and in addition to reduced physical activity includes changes in the hormonal milieu, increased oxidative stress and systemic inflammation, reduced responsiveness to anabolic factors, and decreased protein intake (Figure 1).
The loss of muscle mass with aging, when combined with a concurrent increase in fat mass—termed sarcopenic obesity—results in a particularly adverse combination for physical function and health outcomes. Older adults who are obese (body mass index [BMI] ≥ 30 kg/m2) and have muscle impairment, either defined by low muscle mass or low muscle strength, have accelerated functional decline and an increased risk of morbidity and mortality.8 Recommending weight loss for older adults has been controversial due to research findings showing that relative risk of mortality associated with increased obesity as measured by BMI is actually decreased in older adults.9 Furthermore, the BMI associated with the lowest mortality rate is higher in older adults as compared to young and middle-aged adults.10,11 Nevertheless, disability appears 10 years earlier in individuals who are obese as compared to age-matched individuals who maintain healthy weight, and the increased prevalence of obesity in older adults could lead to an increase in both disability and morbidity.11,12 Using BMI to define obesity in the elderly is frequently criticized on the basis that the two factors used in the equation are affected by age (ie, height is commonly reduced with aging due to vertebral compressions, etc, and weight is influenced by the change in body composition from reduced fat free mass and increased adipose tissue). However, proponents of using BMI argue that it is still the best anthropometric measure to define nutritional status because of the strong relationship with disability, morbidity, and mortality.
In any case, a number of intervention studies have shown that diet-induced weight loss in combination with exercise improves multiple risk factors for coronary heart disease and metabolic syndrome in older adults who are obese.13-16 It should be noted, however, that diet-induced weight loss that is NOT combined with exercise and adequate protein intake leads to further muscle mass loss.
The clinical implications from the evidence presented are that any exercise training programs targeted to older men should be designed to increase and/or maintain muscle mass (hypertrophy and strength) and muscle quality (power, neuromuscular coordination). In addition, the exercise program should be enhanced by other lifestyle modifications that support optimal body composition and help preserve muscle mass. We will discuss these areas in more detail below.
Exercise Training Designed to Increase Muscle Mass, Strength, and Power in Older Men
Resistance training (RT) is very effective in increasing strength in older adults, even in frail elderly persons over the age of 90 years.17,18 Most studies on the effects of RT in older adults have used protocols similar to the ACSM/AHA recommendations (see Table I, #2) and the results show impressive increases in both strength and hypertrophy. However, these improvements have not necessarily translated to improved performance on tasks related to daily function, such as rising from a chair or stair climbing. Although this may be related to studying healthy individuals who are already above the threshold of function, it has also led to the interest in the role of muscle power in physical function and studies on power training in older adults.19,20 It is noteworthy that studies that have compared training programs designed to improve power (using high-velocity movement) to traditional RT protocols for strength have found that the power protocols are just as effective in increasing strength. However, as expected, only the groups performing the power protocol actually improve measures of muscle power.21 The question is, what is the optimal load for increasing muscle power? A study designed to answer this question surprisingly found similar increases in peak leg power using light, moderate, or heavy resistances. The group training with heavy resistance loads had slightly better increases in strength and muscular endurance, as compared to the groups training with moderate or light resistance.22 Another study found that power training in older adults improved balance, especially when performed at low resistance.23 In conclusion, the evidence for using high-velocity, high-intensity RT for improving strength and power in the older adult is compelling. However, proper progression and manipulation of program variables are essential to attain the optimal benefits from RT, including minimizing the risk for injury and limiting training plateaus.
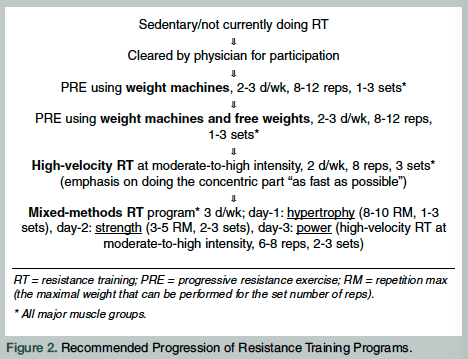
Figure 2 shows the recommended progression in RT from individuals who are naïve to RT to a mixed-methods protocol designed to target different components of muscular function. This progression starts with having the person get accustomed to RT by using weight machines (most gyms will have a dedicated circuit of machines that target all major muscle groups), which are generally regarded as safer to use for a novice and easy to learn. As the person progresses, especially in terms of strength and confidence, free weights are added to the repertoire as an adjunct to the machines. Exercises using free weights generally require more intra- and intermuscular coordination, including the use of stabilizer muscles.24 The next step is to progress into high-velocity power training. This type of training is done with many of the same exercises as used for developing strength and hypertrophy. However, the emphasis is shifted to the speed of the movement. Basically, the person should perform the concentric part (ie, the lifting) of the exercise “as fast as possible.” The speed of the eccentric part (ie, the lowering) should be performed in a controlled manner as to limit the use of momentum in the subsequent repetitions. Using chest press exercise as an example, the pushing out should be done as fast as possible, and then bringing the arms back down should be done in a slower, controlled manner. Further maintenance of muscular function and to keep the program variable can be achieved through a mixed-method RT, where the weekly program varies to specifically target hypertrophy, strength, or power on separate days.25
Other Lifestyle Modifications to Support Optimal Weight and Preservation of Muscle Mass in Older Men
We have primarily emphasized the role of RT in the exercise regimen for older men. However, there are several other important recommendations that the clinician should consider:
1. Weight loss/weight management—The effect of diet (ie, reduction in energy intake) is more important than exercise for achieving initial weight loss. Exercise, however, can help maintain weight loss and prevent weight gain, and is also important for preventing or minimizing the loss of skeletal muscle during the period of the caloric restriction. The recommended approach is to use a modest reduction in energy intake (500-700 kcal/d) and to help the patient set personal goals and identify strategies to improve adherence. Detailed recommendations for weight-loss therapy in the older adult can be found in a position statement of the American Society for Nutrition and The Obesity Society.10
2. Protein intake—Inadequate protein intake results in loss of muscle mass, and many older people do not meet the recommended dietary allowance for protein; most may need even somewhat higher intake to completely meet the metabolic and physiological needs of maintaining skeletal muscle mass.26 The older person is at a particular disadvantage because aging is associated with a reduced responsiveness to both insulin-stimulated and insulin-independent uptake of amino acids in skeletal muscle.27 In order to stimulate muscle hypertrophy and prevent the loss of muscle mass, protein synthesis must exceed protein breakdown. RT, in the absence of feeding, increases both protein synthesis and breakdown, but the net effect is still a negative protein balance. Protein synthesis is stimulated by protein intake via increased availability of amino acids. Additionally, there is a synergistic effect of RT and protein intake on stimulating protein synthesis.28 Therefore, the effects of RT can be maximized by providing adequate protein intake. Timing can also be important, as data suggest that the effects of RT on hypertrophy are even greater when protein is ingested shortly before or after an acute bout of RT.29 Most of the available data indicate that consuming diets with high-quality proteins in adequate (but not excessive amounts) is preferential to using protein-enriched supplements. Both clinicians and patients should know that adequate protein intake (0.8-1.2 g/kg/day) is needed to support protein synthesis for muscle growth. There is no evidence linking protein intake of up to 2 g/kg/day to impaired renal function in healthy men. However, for individuals with significantly impaired renal function, a higher protein diet—especially in animal protein—may be contraindicated.30
3. Aerobic exercise—The benefits of aerobic activity are well recognized and should be an integral part of a well-rounded plan to maintain cardiovascular health, functional capacity, weight management, and to reduce the risk for coronary artery disease, hypertension, diabetes, and other disorders. In addition, aerobic exercise has been shown to reduce oxidative stress31 and partially reverse mitochondrial dysfunction in older men.32 The ACSM/AHA recommendations (Table I) for aerobic activity are a good place to start. The combination of moderate and vigorous activity is, in our opinion, the best strategy because variability (as applied by diverse intensity, duration, and frequency) will result in greater physiological adaptations.
4. When should we advocate “more-is-better”?—As the ACSM/AHA guidelines point out, exceeding the minimum recommended amounts of physical activity will result in higher levels of physical fitness and provide additional health benefits, and may be necessary to help prevent unhealthy weight gain.3 The clinician should be able to recognize the patients who tend to go overboard, as well as the ones who follow the “something-is-better-than-nothing” dogma, and advise accordingly.
What Are the Most Common Exercise-Related Injuries in Older Men?
The most common injuries from exercise participation in older men are acute traumatic injuries such as joint sprains and muscle strains. Overuse injuries can occur from repetitive stress and insufficient rest. Injuries are most likely to occur when the duration, intensity, or frequency of exercise is increased too rapidly instead of allowing a proper progression, and/or from employing an incorrect technique when performing an exercise. The American Academy of Orthopaedic Surgeons recommends using the “10 percent rule,” meaning that the activity level should not be increased by more than 10% per week.33 For example, someone who is currently walking 2 miles a day, 3 days per  week and would like to increase the total weekly distance to 8 miles should do so gradually, and using the 10% rule this increase would take approximately 3 weeks. The 10% rule can also be used as a guide for RT and increasing weights.
week and would like to increase the total weekly distance to 8 miles should do so gradually, and using the 10% rule this increase would take approximately 3 weeks. The 10% rule can also be used as a guide for RT and increasing weights.
One of the most common chronic conditions facing the older population is osteoarthritis of the knee. While many people actually avoid exercise because they fear that it will worsen the osteoarthritis, lack of physical activity can, in fact, make the condition worse and more difficult to live with. RT will help strengthen the muscles around the knee joint, which will lessen the stress on the joint itself. Weight management also plays an important role in protecting the knee joint. If a patient experiences joint discomfort while exercising, it could be due to performing the exercise incorrectly, in which case the technique should be reinstructed and/or he may be advised to do more low-impact exercise to allow the joints to adapt. Table II lists strategies you can share with patients to help them minimize the risk for exercise-related injuries.
The Role of Hormones and Supplements
Some men go to the extremes to maintain youthful appearance and/or abilities. The use of anabolic steroids (most prominently, testosterone), growth hormone, and other performance-enhancing drugs by athletes engaged in competitive sports has been well publicized for nearly half a century. The quest for gaining competitive advantage, however, is as old as the Olympic Games themselves. There are references in Ancient Greek writings to athletes who were found under the influence of performance-enhancing substances and were disqualified from the Games. There is ample evidence that the use (abuse) of very high doses of testosterone and/or other anabolic agents can lead to increased muscle mass and enhanced muscular performance. This unfair competitive advantage was not, however, the main reason that forced the International Olympic Committee to ban the use of these substances. The main reason was the severe risks involved. These include significant increase of cardiovascular and cerebrovascular events, high rates of abnormalities of the reproductive system, and a substantial rise in muscular and skeletal injuries.
Since many older men have low total and/or bioavailable testosterone serum levels, and most have low insulin-like growth factor-1 (IGF-1)/growth hormone, it was believed that restoring their circulating levels might improve the body composition and/or muscular function changes observed with aging. Indeed, nearly 20 years ago, Rudman et al34 reported that short-term administration of growth hormone to older men leads to increased lean body mass and decreased fat mass. This observation has been verified in subsequent larger and/or better controlled studies.35 These favorable body composition changes did NOT lead to better muscular performance. In addition, more than half of these men showed significant side effects, including edema, arthralgias, carpal tunnel syndrome, and impaired glucose tolerance. Furthermore, no data exist on the effectiveness and/or risks of long-term growth hormone administration. Major concerns remain, especially on the risks of diabetes, insulin resistance, and promotion of malignant cell growth.
Similarly, the benefit/risk ratio of long-term testosterone administration is not clear. Several studies have shown that low-dose testosterone replacement is useless. Larger doses can result in increased lean body mass, decreased fat mass, and bone mass improvement. Side effects include benign prostate enlargement, increased prostate-specific antigen, increased hematocrit, and skin allergies. There is no evidence that these body composition changes lead to muscle function improvement. Most well-controlled studies, however, are of limited duration and grossly underpowered for the detection of potential serious side effects such as prostate cancer and cardiovascular event rates (which, in theory, could even be reduced since improved insulin sensitivity has been observed).
Finally, there is no reliable evidence that the use of protein, amino acids, and/or vitamin supplements offers any significant benefit in older men. There are data accumulating that the consumption of whole foods, especially fruits and vegetables, and quality protein sources (eg, fish, eggs, chicken) has far greater beneficial effects than can be achieved through use of supplements.
Summary
Exercise and diet are important tools to prevent or minimize physiological changes associated with aging, to improve general health, and reduce risk of morbidity and mortality. Clinicians may have a unique opportunity to influence their patients’ lifestyle choices. More specific recommendations are likely to have a much greater influence than generic recommendations of “get some exercise and eat healthier.” To summarize, the exercise prescription for older men should include both RT and aerobic exercise. The exercise program should be supported by a healthy diet that includes an adequate amount of quality protein and plenty of fruits and vegetables. We must remember that middle-aged adults who switch to a healthier lifestyle can reduce cardiovascular events by 35% after only 4 years.2
The authors report no relevant financial relationships.
Dr. Traustadóttir is Associate Director of Exercise Sciences, Kronos Longevity Research Institute, Phoenix, AZ, and Assistant Research Professor, Department of Kinesiology, Arizona State University, Tempe; and Dr. Tsitouras is Clinical Director, Kronos Longevity Research Institute.


