Primary MRSA Lung Abscess After Smoke Inhalation
 On the third day of hospitalization for lethargy and respiratory distress after smoke inhalation during a house fire, a 2-month-old girl became febrile, with a temperature of 38.5ºC (101.3ºF). On admission, the infant had a normal white blood cell count and clear breath sounds on auscultation. She had been extubated without complications. Blood, urine, and cerebral spinal fluid culture results were negative. An initial chest radiograph showed subsegmental atelectasis (Figure 1).
On the third day of hospitalization for lethargy and respiratory distress after smoke inhalation during a house fire, a 2-month-old girl became febrile, with a temperature of 38.5ºC (101.3ºF). On admission, the infant had a normal white blood cell count and clear breath sounds on auscultation. She had been extubated without complications. Blood, urine, and cerebral spinal fluid culture results were negative. An initial chest radiograph showed subsegmental atelectasis (Figure 1).
Treatment with intravenous ceftriaxone and clindamycin was started. Over the next 2 days, the infant continued to have fevers, increasing leukocytosis, and decreased breath sounds in the left lower lobe. A second chest radiograph and chest CT scans revealed findings consistent with a lung abscess (Figure 2).
LUNG ABSCESS: AN UNCOMMON COMPLICATION OF PNEUMONIA
A lung abscess is a thick-walled, pus-filled cavity that results from necrosis of lung parenchyma. Primary lung abscesses are known, but uncommon, complications of pneumonia, which can develop after an inhalation injury in a previously healthy child.1 Secondary lung abscesses develop in children with underlying airway or lung pathology, immunologic deficiency, or recurrent aspiration.2 In this patient, airway injury from smoke inhalation and mechanical ventilation led to the development of pneumonia and then a lung abscess.
 Pathogens include aerobic or anaerobic bacteria and fungi. Staphylococcus aureus, group B Streptococcus, Escherichia coli, and Klebsiella pneumoniae should be considered in infants3—and is why this patient was treated with ceftriaxone and clindamycin. Anaerobic bacteria are commonly found in patients with aspiration pneumonia, and fungi are more often associated with infection in immunocompromised patients.
Pathogens include aerobic or anaerobic bacteria and fungi. Staphylococcus aureus, group B Streptococcus, Escherichia coli, and Klebsiella pneumoniae should be considered in infants3—and is why this patient was treated with ceftriaxone and clindamycin. Anaerobic bacteria are commonly found in patients with aspiration pneumonia, and fungi are more often associated with infection in immunocompromised patients.
The estimated incidence of pulmonary abscess in hospitalized children is 0.7 per 100,000.4 Secondary abscesses are more likely to recur as a result of an underlying medical condition, whereas primary lung abscesses are expected to completely resolve.5,6
Clinical course. Lung abscesses develop over several days to weeks, and abnormalities in oxygenation and ventilation may not be apparent early in the course. Typical physical examination findings include fever, tachypnea, decreased air movement, and crackles; however, these findings are also consistent with lobar pneumonia without an abscess and are not always present.3
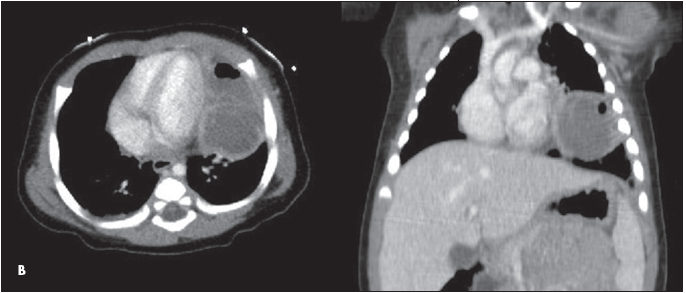 Diagnostic tests. Results of blood and sputum cultures are usually negative; when positive, they can help tailor antibiotic therapy.7 Chest CT scans may be helpful when an air-fluid level is not apparent on chest radiographs.8 MRI has no diagnostic advantage over CT.8
Diagnostic tests. Results of blood and sputum cultures are usually negative; when positive, they can help tailor antibiotic therapy.7 Chest CT scans may be helpful when an air-fluid level is not apparent on chest radiographs.8 MRI has no diagnostic advantage over CT.8
Antibiotic therapy and drainage. Lung abscesses have been treated with long courses of parenteral and enteral antimicrobials based on suspected organisms, with occasional need for lobectomy. CT-guided drainage has become the standard of care, where available, and was performed in this patient on hospital day 6. This approach reduces the duration of fever and symptoms and the length of hospitalization.9 Drainage of lung abscesses also allows for identification of pathogens.
hospital course and patient outcome
In this case, methicillin-resistant S aureus sensitive to clindamycin was isolated. The infant defervesced on day 8 of hospitalization, and inflammatory markers continued to decrease for several more days. She was transitioned to oral clindamycin and completed the recommended 4-week minimum treatment.10


