Rashes and Fever in Children: Sorting Out the Potentially Dangerous, Part 1
Author:
William A. Gibson, MD
Brooke Army Medical Center San Antonio, Texas
Citation:
Gibson WA. Rashes and fever in children: sorting out the potentially dangerous, part 1. Consultant Pediatr. 2008;7(4):141-145.
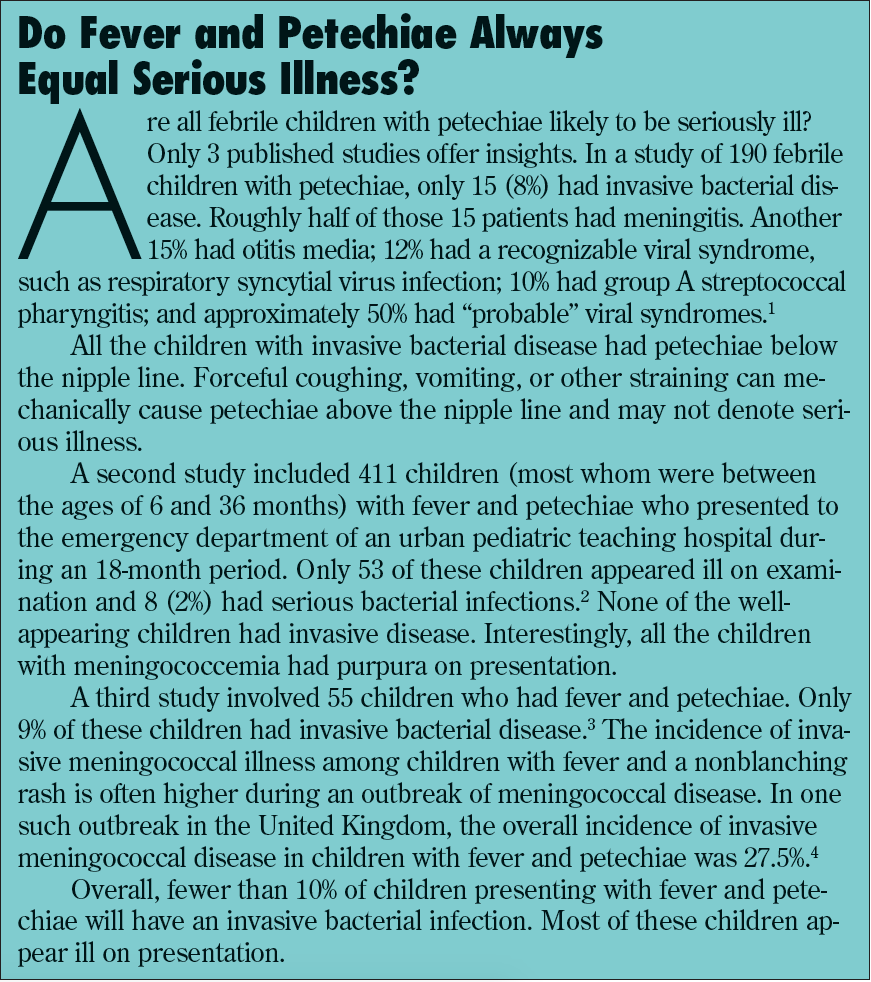
ABSTRACT: Children who present with rash and fever can be roughly divided into 3 groups: the first group includes those with features of serious illness who require immediate intervention. The second and third groups include those with clearly recognizable viral syndromes, and those with early or undifferentiated rash. Here the focus is on those children in group 1 who have petechiae or purpura. The morphology of lesions among children with symptoms of serious illness offers clues to the underlying cause. For example, petechiae may herald such life-threatening disorders as meningococcemia, Rocky Mountain spotted fever, and hemolytic uremic syndrome.
It never fails: your last patient of the day on a Friday is a small child with fever and a rash. This extraordinarily common scenario is one of the most anxiety-provoking and clinically demanding presentations for clinicians. A practical approach to triage can greatly reduce your (and parents') anxiety level and improve diagnostic accuracy.
Children who present with fever and rash fall into 1 of 3 groups:
- Group 1 includes children with features of a recognizable serious illness (Table) who require immediate medical intervention based on the suspected diagnosis.
- Group 2 includes children with clearly recognizable viral syndromes for whom the only required therapy is parental education and reassurance with appropriate follow-up.
- Group 3 includes children who have early or undifferentiated rashes with fever. This group is the largest and most difficult to treat.

Here, in the first of 4 articles, the focus is on those children in group 1 who present with petechiae or purpura and who require your immediate attention. In future issues, I will discuss other febrile rashes that require immediate intervention. I will also focus on rash and fever associated with recognizable viral syndromes and on fever and early or undifferentiated rashes.
NONBLANCHING LESIONS AND FEVER: A COURSE OF ACTION
Life-threatening disorders that present with fever and rash include meningococcemia, other bacterial sepsis or meningitis, Rocky Mountain spotted fever (RMSF), and neoplastic disorders. A discussion of the various rashes associated with neoplastic disorders is beyond the scope of this article.
Nonblanching lesions (petechiae, purpura, and ecchymoses) are defined by their size. Petechiae are less than 2 mm in diameter (Figure 1), purpuric lesions vary from 2 mm to 1 cm, and ecchymoses are larger than 1 cm.

Figure 1. Petechial papules are shown here on the hand of a child with meningococcemia. (Photograph courtesy of Sharon J. Markling, MD, Michael R. Warner, MD, and Charles Camisa, MD)
When a child with a fever and nonblanching lesions appears ill, proceed with a full sepsis evaluation and rapid administration of fluids and broad-spectrum parenteral antibiotic therapy, while arranging transport to the appropriate inpatient setting. If the child appears well and can be monitored, however, I usually elect to observe him or her for a few hours in the office or clinic setting. Most of the life-threatening infections with petechiae are rapidly progressive (Box).1-5 If the child continues to look well and the lesions do not progress, I generally elect to send the child home with close follow-up.
If the nonblanching lesions are widespread, it is prudent to check the platelet count and coagulation factors to rule out idiopathic thrombocytopenic purpura, hemolytic uremic syndrome (HUS), neoplastic disorders, autoimmune disorders, childhood vasculitis syndromes, and other conditions that affect platelet number or function. When you sus suspect HUS, electrolyte levels and renal function must also be evaluated. A more cautious approach is, of course, appropriate when your community is experiencing an increase in the number of invasive meningococcal disease cases.
MENINGOCOCCEMIA
Presentation. Meningococcemia usually begins with a nonspecific febrile prodrome, similar to that of a benign viral process. Later, lethargy, poor appetite, headache, and neck stiffness develop—often with rapid progression to septic shock. Not all patients have petechiae or purpura. In some cases, a maculopapular rash precedes the onset of petechiae. The patient becomes toxic, with tachycardia and hypotension. Disseminated intravascular coagulation, a frequent complication, can lead to diffuse, large, purpuric patches (purpura fulminans). Waterhouse-Friderichsen syndrome refers to adrenal hemorrhage that causes an addisonian crisis. The disease course is rapid, and the outcome is often undesirable.
Between 80% and 85% of patients with invasive meningococcal disease have meningitis, which typically presents with fever, irritability, and headache. Many will also have meningismus and a nonblanching rash. Meningococcal meningitis usually has a milder course and a better prognosis than meningococcal sepsis.6
Keep in mind that not all children with invasive meningococcal disease have a nonblanching rash. In a study of meningococcal disease in Arkansas, of 296 children with invasive infection, 95% presented with fever, 62% had a nonblanching rash, 41% had nuchal rigidity, 41% had hypotension, and 26% required inotropic support and mechanical ventilation.7 The fatality rate in children is 8% to 13%.8 Between 11% and 19% suffer permanent sequelae.9
Wells and colleagues10 evaluated 233 children who presented with fever and petechiae. Those with a fever, purpura, and delayed capillary refill, and who appeared to be ill were most likely to have invasive meningococcal disease. Laboratory evaluation was found to be of little value in determining the diagnosis. However, none of the children with petechiae limited to the distribution of the superior vena cava had meningococcal disease.10
Management. Treatment of patients with suspected meningococcemia includes rapid intravenous access, proper cultures, antibiotic therapy, fluid replenishment, and appropriate pressor support. The preparation of cultures should not delay the initiation of antibiotic therapy.
In addition to Neisseria meningitidis, other bacteria that can cause a similar clinical picture are Haemophilus influenzae and Streptococcus pneumoniae. The initial antibiotic choice should be broad enough to cover all 3 pathogens, unless results of a blood or cerebrospinal fluid Gram stain can guide therapy.
Meningococcal vaccination. Meningococcal disease is associated with 10% to 15% mortality—a rate that has not changed since the 1950s. This disease, which is endemic in the United States, has 2 age peaks: between 6 and 24 months, and in adolescence. The most common serotypes that cause invasive disease are A, B, C, W-135, and Y. A tetravalent polysaccharide vaccine (MPSV4) has been available in this country since 1981; this vaccine is recommended for use in outbreaks and for persons in highrisk groups who are older than 2 years. Polysaccharide vaccines do not produce long-lasting immunity, however, nor do they confer “herd immunity” by decreasing nasopharyngeal carriage.
In January 2005, a meningococcal conjugate vaccine was licensed in the United States for persons aged 11 to 55 years. This vaccine promises longerlasting immunity and should decrease nasopharyngeal carriage. In September 2005, the FDA and the CDC issued an advisory for this vaccine because of a possible link with Guillain-Barré syndrome. This possible association is still being debated, but the American Academy of Pediatrics Committee on Infectious Diseases has not changed its recommendations for administration of this vaccine. Unfortunately, for the single largest age group of persons at risk—ie, children younger than 2 years—the vaccine has not been shown to be efficacious.
In January 2008, Snape and colleagues11 reported promising results with a new meningococcal vaccine that is both well tolerated by and immunogenic in children younger than 2 years. It is a tetravalent vaccine against serogroups A, C, W-135, and Y. The vaccine uses a nontoxic mutant of the diphtheria toxin as a carrier protein and aluminum as an adjuvant. We may see a significant decline in invasive meningococcal disease if further studies confirm these results.
There are still no available vaccines against serogroup B, which accounts for approximately one third of invasive disease in the United States. However, the genome for serogroup B meningococcus has recently been completed and may help researchers identify new strategies for developing an effective vaccine.
ROCKY MOUNTAIN SPOTTED FEVER
Petechiae around the wrists and ankles with fever and headache suggest RMSF (Figure 2). This disease occurs mostly in the southeastern United States but has been reported in 48 states. No cases have been reported in Maine or Vermont.

Figure 2. The spotted rash of Rocky Mountain spotted fever is evident on this child's hand. (Photograph courtesy of the CDC)
The usual incubation period is 5 to 7 days (range, 1 to 15 days). The rash is typically preceded by 2 to 5 days of fever, headache, myalgia, nausea, vomiting, abdominal pain, and jaundice. Hyponatremia is common, and liver function values are often elevated.9
The exanthem usually appears during the second to fourth day of fever and is initially a blanching maculopapular rash. It begins on the thenar eminence and the flexor surfaces of the wrists and ankles and can spread diffusely to involve the entire body. The palms and soles are usually affected. The rash becomes petechial 1 to 3 days after onset. As the disease resolves, the rash may become pigmented and areas of desquamation may appear.
A history of tick bite is helpful but often absent. Bear in mind that roughly 5% to 10% of affected children do not have a rash and that only between 3% and 18% of children with RMSF have a history of rash, fever, and tick bite.12
When the history and physical examination findings are consistent with RMSF, begin presumptive therapy and send biopsy specimens of involved skin or blood to the laboratory for diagnostic confirmation. Blood tests for specific antibodies include indirect hemagglutination, microimmunofluorescence, latex agglutination, enzyme-linked immunosorbent assay, and complement fixation. Results of the most commonly used test, indirect fluorescent antibody, will be negative for the first 4 to 6 days because the infected child has not yet produced sufficient antibodies to the disease. Nevertheless, treatment must be started before this time. When in doubt, send the appropriate tests and treat empirically.
Doxycycline is the drug of choice for children with RMSF. Alternatives include tetracycline and chloramphenicol. In children younger than 10 years, tetracycline can cause teeth discoloration. Doxycycline usually does not have this effect in the doses used for RMSF.13 Chloramphenicol can cause a fatal aplastic anemia and should be reserved for use in pregnant women.14
HEMOLYTIC UREMIC SYNDROME
HUS develops suddenly after a syndrome complex of fever, nausea, vomiting, diarrhea, and abdominal pain. Symptoms of upper respiratory tract infection and ingestion of various medications, such as oral contraceptives, mitomycin, and cyclosporine, have also been temporally related.
Most cases in children are related to an acute gastroenteritis caused by Escherichia coli O157:H7, which produces an endothelial toxin. Unpasteurized milk and inadequately cooked meats are considered the usual means of contamination; however, apple cider and water from swimming pools have also been implicated. Most affected children are younger than 4 years; they often present with lethargy, pallor, and oliguria between 5 and 10 days after the initial GI illness.
In children with HUS, physical examination may reveal dehydration, hepatomegaly, splenomegaly, edema, and petechiae. Affected children are extremely irritable. Laboratory studies show microangiopathic hemolytic anemia, thrombocytopenia, and acute renal failure.15
Although E coli O157:H7 accounts for roughly 80% of cases of HUS in children, other Shiga toxin–producing E coli and non–toxin producing E coli have been implicated—including O26:H11.16 Other causes include Clostridium difficile,17 Shigella, Salmonella, Campylobacter, S pneumoniae, Bartonella, coxsackievirus, echovirus, influenza virus, varicella-zoster virus, Epstein-Barr virus, and HIV. HUS is also associated with systemic lupus erythematosus.
Treatment is supportive and involves early consultation with a pediatric nephrologist for aggressive management of renal failure. The role of antibiotic therapy continues to be explored. However, a meta-analysis of studies performed to date did not show any advantage. While antibiotics do not appear to increase the risk of HUS, most experts avoid their use in this setting.18
Dr Gibson is on the faculty of the San Antonio Uniformed Services Health Education Consortium Emergency Medicine Residency, a joint Air Force and Army program with 46 residents, at Brooke Army Medical Center and Wilford Hall Medical Center in San Antonio, Texas.
REFERENCES:
- Baker RC, Seguin JH, Leslie N, et al. Fever and petechiae in children. Pediatrics. 1989;84:1051-1055.
- Mandl KD, Stack AM, Fleisher GR. Incidence of bacteremia in infants and children with fever and petechiae. J Pediatr. 1997;131:398-404.
- Brogan PA, Raffles A. The management of fever and petechiae: making sense of rash decisions. Arch Dis Child. 2000;83:506-507.
- Banerjee I, Roberts R, Looker N. Incidence of meningococcal infection in children with fever and non-blanching rash. J Infect. 2002;45:275-276.
- Browne BJ, Edwards B, Rogers RL. Dermatologic emergencies. Prim Care. 2006;33:685-695.
- Cartwright KA. Early management of meningococcal disease. Infect Dis Clin North Am. 1999;13:661-684.
- Stovall SH, Schutze GE. Meningococcal infections in children from Arkansas. Pediatr Infect Dis J. 2002;21:366-370.
- Rosenstein NE, Perkins BA, Stephens DS, et al. The changing epidemiology of meningococcal disease in the United States, 1992-1996. J Infect Dis. 1999;180:1894-1901.
- Kirsch EA, Barton RP, Kitchen L, Giroir BP. Pathophysiology, treatment and outcome of meningococcemia: a review and recent experience. Pediatr Infect Dis J. 1996;15:967-979.
- Wells LC, Smith JC, Weston VC, et al. The child with a non-blanching rash: how likely is meningococcal disease? Arch Dis Child. 2001;85:218-222.
- Snape MD, Perrett KP, Ford KJ, et al. Immunogenicity of a tetravalent meningococcal glycoconjugate vaccine in infants: a randomized controlled trial. JAMA. 2008;299:173-184.
- Dantas-Torres F. Rocky Mountain spotted fever. Lancet Infect Dis. 2007;7:724-732.
- Lochary ME, Lockhart PB, Williams WT Jr. Doxycycline and staining of permanent teeth. Pediatr Infect Dis J. 1998;17:429-431.
- Stallings SP. Rocky Mountain spotted fever and pregnancy: a case report and review of the literature. Obstet Gynecol Surv. 2001;56:37-42.
- Razzaq S. Hemolytic uremic syndrome: an emerging health risk. Am Fam Physician. 2006;74:991-996.
- Misselwitz J, Karch H, Bielazewska M, et al. Cluster of hemolytic-uremic syndrome caused by Shiga toxin-producing Escherichia coli O26:H11. Pediatr Infect Dis J. 2003;22:349-354.
- Mbonu CC, Davison DL, El-Jazzar KM, Simon GL. Clostridium difficile colitis associated with hemolytic-uremic syndrome. Am J Kidney Dis. 2003;41:E14.
- Safdar N, Said A, Gangnon RE, Maki DG. Risk of hemolytic uremic syndrome after antibiotic treatment of Escherichia coli O157:H7 enteritis: a meta-analysis. JAMA. 2002;288:996-1001.


