Scabies in Infant and Mother
Photoclinic
Foresee You Next Patient
 The mother of a 3-month-old boy brought her baby for evaluation of a generalized rash of 3 weeks’ duration. She had a similar severely itchy rash on her right shoulder and abdomen. The pruritus was worse at night; the baby seemed fussier at night too. The mother had tried various over-the-counter lotions, with no relief of symptoms.
The mother of a 3-month-old boy brought her baby for evaluation of a generalized rash of 3 weeks’ duration. She had a similar severely itchy rash on her right shoulder and abdomen. The pruritus was worse at night; the baby seemed fussier at night too. The mother had tried various over-the-counter lotions, with no relief of symptoms.
On examination, the infant had a generalized papular, nodular rash that was especially prominent on the neck, axilla, wrist, ankle, and genital area (A and B). Some of the lesions were rather large and erythematous. The mother had a papular, vesicular rash and multiple excoriation marks on her torso and shoulder. Some of the lesions showed early linear tracks and had ulcerated (C).
The baby and his mother have scabies, an intensely pruritic skin infestation caused by Sarcoptes scabiei var hominis. This obligate human parasite is a worldwide public health problem. Although easily treatable, scabies is contagious and the diagnosis is often missed. It is usually transmitted through direct, prolonged contact with an infected person. However, transmission through bedding and clothing may occur because the mites can survive for up to 3 days on such fomites.
 The mites live in the epidermal layers of the skin. As they travel, they secrete proteases and feed on necrotic tissue. The feces (scybala) left behind create the pathognomonic linear lesions. The female mites lay numerous eggs in the deeper layers of the epithelium, while the male mites die after copulation. Less than 10% of the eggs develop into mature mites, and the number of mites a person has is typically less than 100.
The mites live in the epidermal layers of the skin. As they travel, they secrete proteases and feed on necrotic tissue. The feces (scybala) left behind create the pathognomonic linear lesions. The female mites lay numerous eggs in the deeper layers of the epithelium, while the male mites die after copulation. Less than 10% of the eggs develop into mature mites, and the number of mites a person has is typically less than 100.
A type IV hypersensitivity reaction to the mite, its eggs, or its feces develops in the host; this produces severe itching that is the hallmark  of scabies. The reaction typically occurs within 4 to 6 weeks of infestation. Repeated infestations result in hypersensitivity responses that may develop more rapidly (within hours). Scratching the lesions may cause ulceration with secondary bacterial infection.
of scabies. The reaction typically occurs within 4 to 6 weeks of infestation. Repeated infestations result in hypersensitivity responses that may develop more rapidly (within hours). Scratching the lesions may cause ulceration with secondary bacterial infection.
The rash consists of papules, vesicles, pustules, and nodules.1 Adults manifest lesions primarily on the interdigital web spaces of the hands, flexor aspects of the extremities, waist, buttocks, and genitalia. Lesions in infants and small children may be more diffuse. In neonates, who are unable to scratch, an eczematous rash or large nodules may develop. An intensely pruritic rash that is worse at night, that has the classic distribution of lesions, and that is present in other family members should raise suspicion for scabies. In atypical cases, examination of scrapings of the lesions under light microscopy can confirm the diagnosis. This shows the typical 8-legged mites or their eggs (D).
Treatment of scabies must include all family members and close contacts even if they have no symptoms.2 It may be that the hypersensitivity reaction has not developed yet. All clothing and bedding used within the last week should be washed or dry-cleaned after 1 day of treatment and again 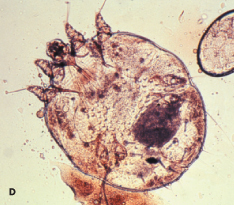 after a week, or they may be sealed in bags for a week. The treatment of choice in children is permethrin 5% cream.3 It is applied all over the body and face for infants, left on for 12 hours, and washed off. This is repeated in 1 week. Lindane 1% cream or lotion, the previous treatment of choice, is no longer used because systemic absorption in children can cause neurotoxicity. In infants younger than 2 months, an alternative therapy is 6% sulfur in petrolatum for 3 consecutive 24-hour periods. Widespread infestations in institutions may be treated with oral ivermectin; however, this agent is not approved for use in children younger than 5 years. Symptomatic treatment with oral antihistamines and topical antipruritics or corticosteroids may be necessary even after the mite is eliminated because of persistent hypersensitivity to the dead mite and its feces.
after a week, or they may be sealed in bags for a week. The treatment of choice in children is permethrin 5% cream.3 It is applied all over the body and face for infants, left on for 12 hours, and washed off. This is repeated in 1 week. Lindane 1% cream or lotion, the previous treatment of choice, is no longer used because systemic absorption in children can cause neurotoxicity. In infants younger than 2 months, an alternative therapy is 6% sulfur in petrolatum for 3 consecutive 24-hour periods. Widespread infestations in institutions may be treated with oral ivermectin; however, this agent is not approved for use in children younger than 5 years. Symptomatic treatment with oral antihistamines and topical antipruritics or corticosteroids may be necessary even after the mite is eliminated because of persistent hypersensitivity to the dead mite and its feces.
This baby and his mother were treated with permethrin 5% cream. They returned after a week with significant reduction in the rash and itching and were reassured that these symptoms would gradually resolve. ■
1. Johnston G, Sladden M. Scabies: diagnosis and treatment. BMJ. 2005;331:619-622.
2. Chambliss ML. Treating asymptomatic bodily contacts of patients with scabies. Arch Fam Med.2000;9:473-474.
3. Zargari O, Golchai J, Sobhani A, et al. Comparison of the efficacy of topical 1% lindane vs 5% permethrin in scabies: a randomized, double-blind study. Indian J Dermatol Venereol Leprol. 2006;72:33-36.


