Why Does This Preteen Have Hip Pain?
A 12-year-old boy presented to the orthopedic clinic with a 3-week history of left hip pain that began after he was tackled at a school football game. After the football injury, the boy was taken to an emergency facility where knee and hip radiographs were conducted, both with unremarkable results. He was given ibuprofen and crutches, discharged, and referred to an orthopedist. In the orthopedic clinic, he reported that 3 months prior to the football incident, he had noticed left knee pain for a few days, but the pain had since resolved. However, he denied having fever or pain in other joints at the present time. His physical examination results were notable for a weight of 55.8 kg (90th percentile), a body mass index of 26.6 (97th percentile), and external rotation of the left leg while supine. When the boy stood on the affected leg, the gluteal fold on the unaffected side fell instead of rising, indicating a positive Trendelenburg sign. An anteroposterior (AP) radiograph of the boy’s hip was obtained (Figure 1).

What is the cause of the boy’s symptoms?
(Answer and explanation on the next page.)
Answer: Slipped capital femoral epiphysis
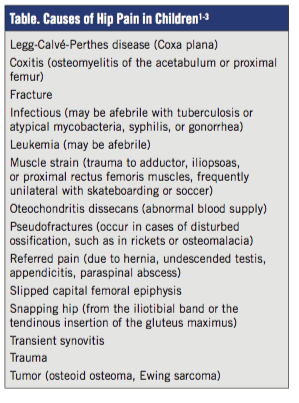
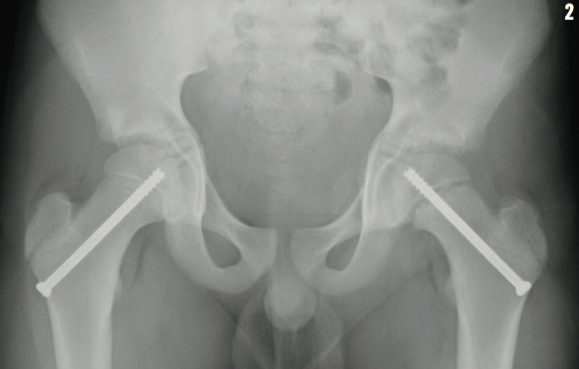
Hip pain in children can indicate a variety of possible diagnoses (Table).1-3 In our patient, the AP radiograph of the hip showed a Type 1 Salter-Harris fracture, or slipped capital femoral epiphysis (SCFE), of the left physis. The boy underwent surgical pinning of the affected and unaffected hips the next day (Figure 2).
SCFE is a fracture through the proximal femoral growth cartilage; the femoral epiphysis is displaced posteriorly and inferiorly relative to the metaphysis. In children aged 8 to 15 years, the incidence of SCFE is 0.33 per 100,000 to about 24 per 100,000, with a peak incidence at 11 years of age for girls and 13 years of age for boys. SCFE occurs during the adolescent growth spurt when growth plates are most vulnerable to shearing forces, and it is 3 times more common in boys, possibly due to the weakening effect of testosterone on the physis.4,5
Seventy-five percent of SCFEs are unilateral. Hip pain and limping are common, but pain in the knee or groin can also occur. At rest, hip flexion and external rotation are favored due to the new anatomic geometry formed by the slip.5,6 The frog-leg lateral radiograph best shows the posterior slippage, and the AP view shows widening of the growth plate and rarefaction of the adjacent metaphysis.4,7
Most slips occur slowly over many months, but gradual and acute components, as in our patient, may be present. While trauma and endocrine disorders such as hypothyroidism, hypopituitarism, and hypogonadism are important risk factors, slips are most commonly associated with obesity.8,9 However, the risk may be reversible; obese children with a unilateral SCFE who become nonobese decrease their odds of a contralateral SCFE.9,10
The aim of management is to prevent further slipping and complications such as avascular necrosis and osteoarthritis, and this is usually achieved by percutaneous pinning.5 Our patient underwent prophylactic pinning of the normal hip.11 This procedure carries some risk of avascular necrosis, chondrolysis, and fracture, but approximately 24% of untreated patients can develop a contralateral SCFE within 18 months.12 Factors such as age, obesity, follow-up ability, and contralateral radiography findings support preventative intervention.13 After surgery, the patient resumed full weight bearing and returned to football after 6 months.
Joshua Jones, BS; Alex Tse, BS; and Lynnette Mazur, MD, MPH, are with the University of Texas Health Science Center at Houston.
REFERENCES
1. Mont MA, Cherian JJ, Sierra RJ, Jones LC, Lieberman JR. Nontraumatic osteonecrosis of the femoral head: where do we stand today? J Bone Joint Surg Am. 2015;97(19):1604-1627.
2. Kocher MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis and transient synovitis of the hip in children: an evidence-based clinical prediction algorithm. J Bone Joint Surg Am. 1999;81(12):1662-1670.
3. Serner A, Tol JL, Jomaah N, et al. Diagnosis of acute groin injuries: a prospective study of 110 athletes. Am J Sports Med. 2015;43(8):1857-1864.
4. Loder RT, Skopelja EN. The epidemiology and demographics of slipped capital femoral epiphysis. ISRN Orthop. 2011;2011:486512.
5. Staheli LT. Fundamentals of Pediatric Orthopedics. 4th ed. Philadelphia, PA: Wolters Kluwer/Lippincott Williams & Wilkins; 2008.
6. Fleisher GR, Ludwig S, Henretig FM. Textbook of Pediatric Emergency Medicine. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006.
7. Wu GS, Pollock AN. Slipped capital remoral epiphysis. Pediatr Emerg Care. 2011;27(11):1095-1096.
8. Compton S. Childhood obesity and slipped capital femoral epiphysis. Radiol Technol. 2014;85(3):321CT-326CT.
9. Nasreddine AY, Heyworth BE, Zurakowski D, Kocher MS. A reduction in body mass index lowers risk for bilateral slipped capital femoral epiphysis. Clin Orthop Relat Res. 2013;471(7):2137-2144.
10. Verdeja-Morales E, Zavala-Morales A, Gómez-Gutiérrez FJ, Rojo-Tierradentro G. Slipped proximal femoral epiphysis in adolescents. Risk factors. Acta Ortop Mex. 2012;26(1):3-9.
11. Popejoy D, Emara K, Birch J. Prediction of contralateral slipped capital femoral epiphysis using the modified Oxford bone age score. J Pediatr Orthop. 2012;32(3):290-294.
12. Sankar WN, Novais EN, Lee C, Al-Omari AA, Choi PD, Shore BJ. What are the risks of prophylactic pinning to prevent contralateral slipped capital femoral epiphysis? Clin Orthop Relat Res. 2013;471(7):2118-2123.
13. Riad J, Bajelidze G, Gabos PG. Bilateral slipped capital femoral epiphysis: predictive factors for contralateral slip. J Pediatr Orthop. 2007;27(4):411-414.


