Discordant ECG Findings in a Man With Chest Pain
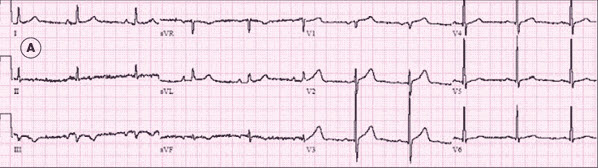
An 80-year-old man presents to the emergency department (ED) with intermittent dyspnea and chest pain. He has hypertension and osteoarthritis but no known cardiac disease. Vital signs are normal. No jugular venous distention is noted. The lungs are clear with equal breath sounds, and the heart rate is regular, without murmurs, gallops, or rubs. The chest wall is not tender. No edema or asymmetry is evident in the extremities. The initial ECG (A) is shown above.
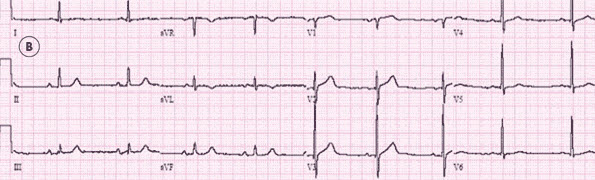
While he is in the ED, his chest pain and dyspnea resolve spontaneously. A second ECG (B) is obtained.
Which of the following best explains the ECG findings?
A. Anteroseptal myocardial ischemia.
B. Inferior myocardial ischemia.
C. Lateral myocardial ischemia.
D. Pulmonary embolism.
E. Limb electrode reversal.

What's Your Diagnosis?
CORRECT ANSWER: E
WHAT THE ECG SHOWS
The first ECG (Figure 1) shows normal sinus rhythm at roughly 60 beats per minute. The axis is normal (the principal QRS vector is upright/ positive in leads I and aVF), and the intervals are normal as well. How-ever, T-wave inversion is evident in leads III and aVF (2 contiguous inferior leads). This invokes a wide differential diagnosis (Table).1
Narrowing the differential. The second ECG (Figure 2) was obtained after the patient's chest pain and dyspnea had resolved. The rate and rhythm are unchanged. If the tracing is scanned for signs of dynamic ischemic change, it is evident that the inverted T waves in leads III and aVF and the relatively flattened T wave in lead II in Figure 1 are now upright. These changes suggest inferior myocardial ischemia (B).

However, the T waves that were upright in leads I and aVL in the first tracing are now flat (lead I) or inverted (lead aVL), arousing suspicion of lateral myocardial isch-emia (C). The lateral precordial leads (V5 and V6) are static and appear normal in both tracings, which casts some doubt on the possibility of lateral ischemia. Nonetheless, coronary ischemia remains high on the differential diagnosis.
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
The normal appearance of—and absence of change in—precordial leads V1 through V4 on both ECGs rules out acute anteroseptal myocardial ischemia (A). It could be argued that lead V1 features a QS complex, which might signal age- indeterminate septal myocardial infarction; however, the absence of an accompanying QS complex in lead V2 makes this unlikely.
Pulmonary embolism (D) can present with myriad nonspecific ECG changes—including sinus tachycar- dia, atrial fibrillation, complete and incomplete right bundle-branch block, S1Q3T3, P pulmonale, anterior T-wave inversion, global T-wave inversion, ST-segment changes, and QRS-axis changes—or a normal ECG. Thus, these 2 ECGs in a patient with chest pain and dyspnea are consistent with pulmonary embolism; moreover, sinus tachycardia is commonly absent in patients with pulmonary embolism, as it is in this man.2,3
Because the differential diagnosis still includes both coronary isch-emia and pulmonary embolism—and anterior ischemia is the only condition that appears truly unlikely—the next step is to look for findings in the tracings that could help "rule in" a diagnosis.
QRS-axis changes. Pulmonary embolism may present with a change in the QRS frontal plane axis; thus, a determination of the QRS axis should be made on both of this patient's tracings. Ballpark QRS-axis determinations are easily made by ascertaining which of the 4 possible quadrants—normal, left, right, or extreme—a tracing reveals. Determination of the precise QRS axis in the frontal plane is arguably not necessary on every ECG, especially since the computer reading usually provides an accurate determination of the QRS axis.
According to the computer, these tracings demonstrate a shift in QRS frontal plane axis from +4° (Figure 1) to +50° (Figure 2). Visual inspection of the ECGs shows that the principal QRS vector in lead I is upright in both tracings. However, the QRS complex in lead aVF is near-isoelectric in Figure 1 (ie, the axis is around 0°, because lead I is upright) and plainly positive in Figure 2 (somewhere between 0° and +90°—more precisely, somewhere near +60°, because lead aVL is the closest to being isoelectric, and its vector of 230° is perpendicular to a +60° vector). Further scrutiny reveals that the QRS complex in lead III in the first tracing is directed downward (as is the T wave in the same lead), but in the second tracing, it is directed upward.
What could be causing these changes? Although pulmonary embolism could be responsible for these axis changes, they are also consistent with another, nonpathological entity: limb electrode reversal (E).
LEFT ARM/LEFT LEG ELECTRODE REVERSAL
The changes seen on this patient's ECGs are the result of inadvertent reversal of the left-sided limb electrodes—that is, the left arm (LA) electrode has been placed on the left leg, and the left leg (LL) electrode has been connected to the left arm. This is the most difficult of the limb electrode reversals to detect.4,5 The difficulty stems from the fact that reversal of these 2 electrodes does not give the ECG a blatantly abnormal appearance; in fact, it results in parallel changes in lead display.
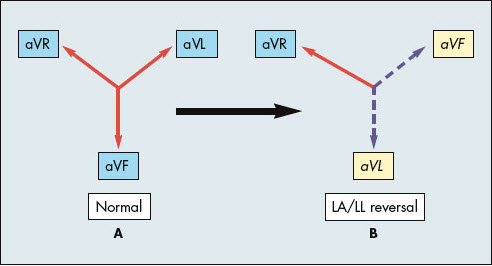
 Detection of electrode reversal begins with recollection of normal lead vector configuration (Figure 3). Reversing the LA and LL electrodes gives rise to changes in lead I (which then displays lead II complexes), lead II (which then displays lead I complexes), and lead III (which then displays the old lead III complex, but inverted) (Figure 4). The augmented leads are similarly affected: the waveforms displayed in lead aVF become those displayed in lead aVL—and vice versa—while lead aVR is unaffected (Figure 5). In summary, 2 inferior leads (II and aVF) wind up in a lateral position (I and aVL), and 2 lateral leads (I and aVL) are switched to an inferior position (II and aVF). Lead III is simply inverted—something that does not catch the eye of most clinicians who read ECGs because of the normal wide variability in the QRS vectors of lead III.6
Detection of electrode reversal begins with recollection of normal lead vector configuration (Figure 3). Reversing the LA and LL electrodes gives rise to changes in lead I (which then displays lead II complexes), lead II (which then displays lead I complexes), and lead III (which then displays the old lead III complex, but inverted) (Figure 4). The augmented leads are similarly affected: the waveforms displayed in lead aVF become those displayed in lead aVL—and vice versa—while lead aVR is unaffected (Figure 5). In summary, 2 inferior leads (II and aVF) wind up in a lateral position (I and aVL), and 2 lateral leads (I and aVL) are switched to an inferior position (II and aVF). Lead III is simply inverted—something that does not catch the eye of most clinicians who read ECGs because of the normal wide variability in the QRS vectors of lead III.6
 Suspect inadvertent limb electrode reversal when ECG changes are surprising given the clinical scenario. Suspect LA/LL reversal in particular when 2 tracings from the same patient demonstrate an unexpected shift in the QRS axis and closer scrutiny reveals that between the first and second tracings, leads I and II have been reversed, leads aVL and aVF have been reversed, and lead III has become inverted. To determine which tracing is correct, repeat the ECG with close attention to proper electrode placement.
Suspect inadvertent limb electrode reversal when ECG changes are surprising given the clinical scenario. Suspect LA/LL reversal in particular when 2 tracings from the same patient demonstrate an unexpected shift in the QRS axis and closer scrutiny reveals that between the first and second tracings, leads I and II have been reversed, leads aVL and aVF have been reversed, and lead III has become inverted. To determine which tracing is correct, repeat the ECG with close attention to proper electrode placement.
In most cases, evidence of LA/LL reversal can also be detected on a single tracing. One series of 70 cases of LA/LL electrode reversal found 2 P-wave characteristics that accurately identified this misconnection in 90% of patients. Thus, if the ECG either demonstrates a larger P-wave amplitude in lead I than in lead II or shows a terminal positive component of the P wave in lead III, LA/LL electrode reversal is probable.5
 These criteria are easier to remember if normal atrial depolarization vectors are considered. On a normal ECG, the P wave is usually larger in lead II than in lead I because the normal P-wave axis is between +45° and +60°—that is, it more closely approximates the vector of lead II (+60°) than that of lead I (0°). Furthermore, lead III has a rightward vector (+120°); thus, one would expect a biphasic P wave in lead III to have an initially upward deflection followed by a downward deflection (because the right atrium is depolarized before the left). A terminally positive P wave in a right-sided lead is unusual.
These criteria are easier to remember if normal atrial depolarization vectors are considered. On a normal ECG, the P wave is usually larger in lead II than in lead I because the normal P-wave axis is between +45° and +60°—that is, it more closely approximates the vector of lead II (+60°) than that of lead I (0°). Furthermore, lead III has a rightward vector (+120°); thus, one would expect a biphasic P wave in lead III to have an initially upward deflection followed by a downward deflection (because the right atrium is depolarized before the left). A terminally positive P wave in a right-sided lead is unusual.
OUTCOME OF THIS CASE
The discrepancy between the 2 ECGs was detected in the ED, and limb electrode reversal was suspected. A third ECG with close attention to proper electrode placement was obtained; it established that the first tracing contained the LA/LL reversal. Of note, the tracing in Figure 1 has a larger P wave in lead I than in lead II—a telltale sign of LA/LL electrode reversal.
The patient was admitted for further workup of his chest pain. Cardiac enzyme levels were normal. Myocardial infarction was ruled out, and he was discharged without a definitive diagnosis.
1. Brady WJ. T wave. In: Chan TC, Brady WJ, Harrigan RA, et al, eds.ECG in Emergency Medicine and Acute Care. Philadelphia: Elsevier Mosby; 2005:66.
2. Daniel KR, Kline JA. Pulmonary embolism. In: Chan TC, Brady WJ, Harrigan RA, et al, eds. ECG in Emergency Medicine and Acute Care. Philadelphia: Elsevier Mosby; 2005:288.
3. Chan TC, Vilke GM, Pollack M, Brady WJ. Electrocardiographic manifestations: pulmonary embolism. J Emerg Med. 2001;21:263.
4. Surzwicz B, Knilans TK. Chou's Electrocardiography in Clinical Practice. 5th ed. Philadelphia: WB Saunders; 2001.
5. Abdollah H, Milliken JA. Recognition of electrocardiographic left arm/left leg lead reversal. Am J Cardiol. 1997;80:1247.
6. Harrigan RA. Electrode misconnection, misplacement, and artifact. Emerg Med Clin N Am. 2006;24:227.


